Advanced critical care echocardiography case review by Hassan Raza M.D.
Suggested material to watch before this: https://www.youtube.com/watch?v=UrQKyURqDBI
Cited in the video:
SHOCK trial: https://doi.org/10.1016/s0002-9343(00)00310-7
Contemporary Management of Cardiogenic Shock: https://doi.org/10.1161/cir.0000000000000525
Principles of Doppler
Learn the principles of Doppler ultrasound in this 20-minute screencast from Dr. Katie Wiskar. This tutorial covers basic ultrasound physics, different Doppler modes, and multiple examples from various POCUS applications.
Relevant Screencasts
Tutorial on aortic stenosis vs sclerosis: https://westernsono.ca/aortic-stenosis-vs-sclerosis/
Tutorial on transcranial Doppler: https://westernsono.ca/screencasts/miscellaneous/trans-cranial-doppler-tcd/
Tutorial on calculating stroke volume using LVOT VTI: https://westernsono.ca/screencasts/echo/stroke-volume-determination/
Greetings POCUS people!
The weather finally seems to have calmed down (this westcoast girl has been sweltering in the humidity – bring on the rain!), the leaves are turning, and the smell of pumpkin spice lattes fills the air. It’s officially fall – a whole new season of POCUS goodness.
The Case
This is a 69-year old male post-PEA arrest admitted with severe pancreatitis and ARDS. He very sick, on substantial doses of three vasopressors. Oxygenation/ventilation has also been a challenge, and he’s consequently on high levels of PEEP. The fellow comes over, scalpel in hand – does this guy need a chest tube?
COTG
This 67-year old lady is admitted to the unit with a GI bleed and suspected sepsis. Without giving too much away, I’ll say that she has a significant cardiac PMHx that was concerning for being a major cause of her shock. Based on these images, what can you say about the etiology of her ongoing shock?
Eye (s)Candy
Sometimes you don’t necessarily want to learn; you just want to look at beautiful POCUS pictures. Introducing our new Eye (s)Candy (get it?) feature – for those clips that are just too pretty not to stare at.
If anyone needs me this week, I’ll be sitting here hypnotized by the intoxicating bubbles in this right atrium – shown beautifully on a TEE bubble study.
Answer to Last Weeks Case
For the ultrasound terminology nerds, this one’s a real winner. We have no less than THREE specific “signs” identifiable in this particular clip.
Most of you will have correctly identified a large pleural effusion (the anechoic space), seen above the liver and diaphragm (screen right). There is collapsed atelectatic lung flapping around inside the effusion – termed the Jellyfish sign (1). We also see spine inferior to the effusion, which is not normally visible in the thorax through aerated lung – the Spine sign (2).
Finally, the astute among you will have picked up the swirling debris in the inferior aspect of the effusion. You’ll note how the effusion goes from completely anechoic more anteriorly, and then gradually becomes more isoechoic in a ombre-like manner (the effusion is very on-trend). This is seen in hemorrhagic effusions due to gravitational layering of cellular and liquid components of blood, the same way blood will separate in a test tube if left long enough. It’s termed the Hematocrit sign (3), and is very useful when seen to identify blood within a space.
In this patient’s case, she had a hemorrhagic pleural effusion secondary to her metastatic malignancy. A chest tube was placed for drainage and she experienced symptomatic relief.
Answer to Last Weeks COTG
This is a very interesting case where spectral Doppler beautifully illustrates dynamic physiology changes that otherwise may have gone unnoticed. POCUS for the major win.
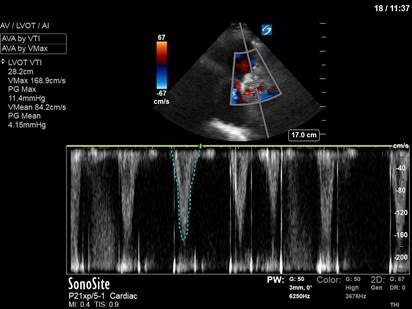
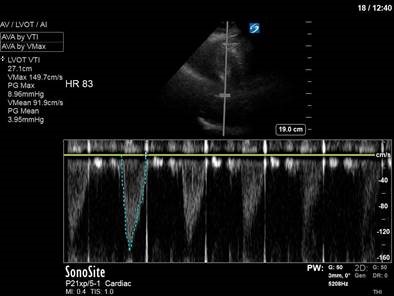
In the initial A4C clip, you can appreciate that the heart appears hyperdynamic, with the LV walls seeming to touch in systole. Putting PW though the LVOT to get our VTI revealed aliasing, meaning that the velocities in that location exceed our Nyquist limit and can’t be processed.
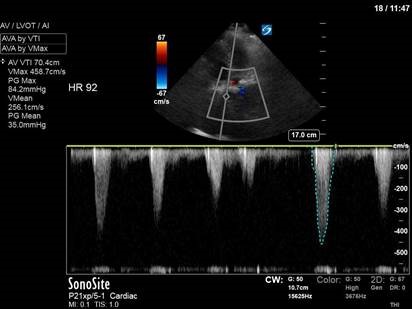
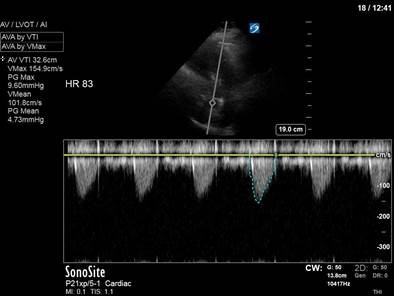
Our next image uses spectral doppler in the same location, but CW instead of PW. This time we are able to measure the maximal velocity and pressure gradient (remember, CW has no Nyquist limit), which reveals a maximum pressure gradient of 45, and a mean pressure gradient of 21. VTI measured here would be 61 – CRAZY high.
So what’s causing these sky-high numbers? Something has caused blood flow to speed up – significantly – though the LVOT. Very high LVOT VTI readings should always make you suspicious for some sort of intra-cavitary gradient or obstruction. In her case, a significant pressure gradient is obviously present. With a very keen eye (and a clip played at 1/4 speed), you can actually appreciate the anterior leaflet of the mitral valve being pulled towards the septum in systole – aka SAM (systolic anterior motion of the mitral valve), most commonly seen in HOCM, and associated with LVOT obstruction.
In our patient’s case, there was no history of hypertrophic cardiomyopathy, and she had a fairly normal pre-op echo. However, the combination of an underfilled LV (secondary to hemorrhagic shock and incomplete resuscitation) and hyperdynamic contractility (with the addition of the dobutamine) led to transient LVOT obstruction.
The POCUS crew quickly advised the ICU team of our findings. Dobutamine was discontinued, and the patient was further resuscitated. A repeat POCUS study was done the next day, with the patient now weaned off all inotropes or vasopressors:
Often these patients will have underlying substrate that predisposes them to transient LVOT obstruction, such as LVH or a sigmoid septum; though none seem to be obviously present in our patient (septum is just slightly sigmoid-shaped).
See the attached paper for a discussion of dynamic LVOT obstruction in the setting of catecholamine use. It’s not frequently diagnosed, but is something that should be considered in all patients who worsen with initiation of inotropic therapy.
dynamic LVOTobs catecholamines
Happy scanning!
The POCUS team
CCW POCUS crew has been hard at work and would like to welcome this months’ rotators Dr. Kimberley Lewis, Mo Dairi, and Steve Roy. They will be providing some of the COTW cases over the next few weeks (we hope!).
This weeks case comes from Drs. Fulan Cui and Scott Anderson. We’ll leave the interpretation and critique of Andersons POCUS skills to you (but feel free to reply-all… just saying!)
The Case:
70’s F with known severe aortic stenosis and CAD was admitted to hospital with progressive shortness of breath and was awaiting cardiac surgery. She was brought to CSRU with refractory hypotension, and a POCUS was completed to assist in shock differentiation. Here is one clip: What are we looking at? What is your differential for what this might be?
Last Weeks Case:
This clip comes from a DVT study. This image was captured using a linear probe on the vascular setting. With the probe marker oriented towards the patients’ right side, we can tell that this is the right leg (NAVY remember? the vein will always be on the same side as the limb). POCUS DVT studies are performed using compressive ultrasonography. In general, depth should be adjusted to see both artery and vein as we see here. Assess the 2D image for apparent clot or thrombus and if nothing is visible apply direct vertical pressure to assess for compressibility. The vein should be compressible when applying less pressure than necessary to compress the adjacent artery. Several anatomic regions need to be assessed, please refer to your favorite POCUS reference for an in-depth review of required anatomy. This clip, taken at the level of the lateral perforator demonstrates clear clot within the vein, and so no compression was applied. This patient went on to be diagnosed with DVT and was placed on therapeutic anticoagulation.
Hope you enjoyed today’s installment of COTW,
The POCUS Team
Welcome to our newest rotators: Ali AlHarbi, Mike Beyea, and Zainab AlDuhalib who will be providing you with COTW material for Block 12.
The Case:
Without any clinical context – can you guess what type of patient this clip might be from? What abnormalities can you spot?
COTG:
Same patient, what are we assessing for here?
Answer from Last Week:
Last week we presented the case of a 62-year-old gentleman requiring paracentesis. To guide paracentesis a high-frequency linear probe was used to generate the first image of the abdominal wall in the near field with ascitic fluid in the far field. The next still image depicts measurements approximating how thick the abdominal wall is, and how much fluid lies beneath. This offers the proceduralist an estimate of how far the needle should be advanced before fluid will return. Finally, colour Doppler has been used to assess for vessels – most importantly to check for the presence of the inferior epigastric artery which could lead to significant bleeding if lacerated or punctured. The third clip demonstrates pulsatile colour flow, indicating the presence of a vessel and necessitating a different location for paracentesis. Look for the upcoming CHEST article Better with ultrasound – Paracentesis for more info (currently article in press)
The Clip-of-the-Geek:
Also acquired with the linear probe, these clips depict the diaphragm of a patient with a C-spine injury following MVC while he is spontaneously breathing on a trach mask trial. Diaphragm assessment in the critically ill generally involves two measurements: Diaphragm excursion, and thickening. To measure thickening (what we’ve done here), use a high-frequency transducer to locate the diaphragm, which appears as a three-layered structure (diaphragmatic layers of pleural and peritoneal pleura, and a middle hyperechoic layer of muscle). From here use M-mode to take caliper measurements of diaphragmatic thickening at end inspiration, and end expiration. Thickening fraction = (end inspiratory thickness – end expiratory thickness)/end expiratory thickness. Diaphragm assessments in critically ill are very complex and will depend on the patients’ sedation levels, injuries, ventilatory support, etc. In this case, the fact that the diaphragm was moving, and thickening was helpful to rule out diaphragmatic paralysis due to high C-spine injury.
Until next time!
The POCUS Team
A sol d out CRUS 2017 brought new teaching strategies and continued legacy of training cutting edge point-of-care ultrasound techniques to a broad cross section of physicians. Residents and consultants from 8 different specialties took to University Hospital in the middle of August to begin the journey to ultrasound mastery in point-of-care techniques such as lung, cardiac and abdominal ultrasound.
d out CRUS 2017 brought new teaching strategies and continued legacy of training cutting edge point-of-care ultrasound techniques to a broad cross section of physicians. Residents and consultants from 8 different specialties took to University Hospital in the middle of August to begin the journey to ultrasound mastery in point-of-care techniques such as lung, cardiac and abdominal ultrasound.
This course marked the introduction of a series of new innovations. We unveiled a new 3rd day of simulation enriched ultrasound teaching, lead by Dr. Rob Leeper. We also launched an inaugural retention strategy following the course that will allow participants to continue to receive mentorship and support following the course to ensure they sustain and grow their skills.
Timing and location of CRUS 2018 to be announced but please stay tuned and check www.resus.us regularly.
See a full repository of images from the course here.
]]>www.resus.us
The 2 day course (with the option of a 3rd half-day) is being held on August 16th, 17th (and 18th) 2017 at the sophisticated CSTAR facility at University Hospital in London, Ontario. This is the biggest and most comprehensive course of its kind offered in Canada. It is ideal for any clinician involved in resuscitation, such as intensivists, emergency physicians, anesthesiologists or internists.
In the core 2-day course, we emphasize resuscitative ultrasound in the following domains:
-critical care echocardiography
-lung and pleural ultrasound
-abdominal free fluid
-ultrasound guided vascular access (central, peripheral and arterial lines)
-DVT
For those who wish to stay for the 3rd day, a half-day ultrasound enriched simulation experience run by our local sim experts.
NEW this year – we have a new “retention” package that is looking to help those physicians working without much ultrasound mentorship to retain their skills after the course through regular video conference sessions for the year following our course. Be sure to check out all the different registration options on our course website.
]]>The Division of Emergency Medicine is once again pleased to host its annual “Introduction to ED Point of Care Ultrasound” course on July 6th, 2017.
This course will emphasize fundamental techniques in image acquisition and interpretation and 7 indications of point of care ultrasound in the ED. Course content is aimed at practitioners who are beginning their pathway to competence in point of care ultrasound.
Topics covered will be:
- Abdominal : Presence of intra-peritoneal fluid? (Yes/No)
- Abdominal : Presence of abdominal aortic aneurysm? (Yes/No)
- Subcostal Cardiac : Presence of pericardial fluid? (Yes/No) Cardiac activity during arrest? (Yes/No)
- Pelvic : Presence of an intra-uterine pregnancy? (Yes/No)
- Thoracic: Presence of pneumothorax (Yes/No) Presence of a pleural effusion (Yes/No)
The course will feature an outstanding faculty to learner ratio for hands-on sessions as well as innovative image interpretation sessions. These small group sessions emphasize image interpretation skills and serve as intimate venues to reinforce clinical integration pathways.
Course director is Dr. Heather Hames. Bedside instructors will include faculty from within the Division of EM’s experienced group of point of care sonographers.
If you have interest in attending as a participant please contact us via email at [email protected] (please include Emergency Course in subject line).
Last years course filled up quickly so please contact us if interested.
Some pics from our previous courses can be found here.
]]>The Division of Emergency Medicine is once again pleased to host its annual “Introduction to ED Point of Care Ultrasound” course on July 6th, 2017.
This course will emphasize fundamental techniques in image acquisition and interpretation and 7 indications of point of care ultrasound in the ED. Course content is aimed at practitioners who are beginning their pathway to competence in point of care ultrasound.
Topics covered will be:
- Abdominal : Presence of intra-peritoneal fluid? (Yes/No)
- Abdominal : Presence of abdominal aortic aneurysm? (Yes/No)
- Subcostal Cardiac : Presence of pericardial fluid? (Yes/No) Cardiac activity during arrest? (Yes/No)
- Pelvic : Presence of an intra-uterine pregnancy? (Yes/No)
- Thoracic: Presence of pneumothorax (Yes/No) Presence of a pleural effusion (Yes/No)
The course will feature an outstanding faculty to learner ratio for hands-on sessions as well as innovative image interpretation sessions. These small group sessions emphasize image interpretation skills and serve as intimate venues to reinforce clinical integration pathways.
Course director is Dr. Heather Hames. Bedside instructors will include faculty from within the Division of EM’s experienced group of point of care sonographers.
If you have interest in attending as a participant please contact us via email at [email protected] (please include Emergency Course in subject line).
Last years course filled up quickly so please contact us if interested.
Some pics from our previous courses can be found here.
]]>
The 7th annual Canadian Resuscitative Ultrasound Course (formerly Critical Care Ultrasound Course) is now open for registration!
(download the brochure for the course here)
The 2 day course (with the option of a 3rd half-day) is being held on August 18th, 19th (and 20th) 2016 at the sophisticated CSTAR facility at University Hospital in London, Ontario. This is the biggest and most comprehensive course of its kind offered in Canada. It is ideal for any clinician involved in resuscitation, such as intensivists, emergency physicians, anesthesiologists or internists.
In the core 2-day course, we emphasize resuscitative ultrasound in the following domains:
-critical care echocardiography
-lung and pleural ultrasound
-abdominal free fluid
-ultrasound guided vascular access (central, peripheral and arterial lines)
-DVT
For those who wish to stay for the 3rd day, a half-day workshop will focus on more advanced echocardiographic techniques including:
-determination of stroke volume
-quantitative right sided assessment
-valvular assessmentBrochure for ccus 2016 Final
-goal directed TEE
Images from last year’s course:
The course is designed to maximize time spent engaged in practical skills like scanning or practicing image interpretation:
-exceptional participant to faculty ratio of 2:1 for bedside scanning instruction
-lecture content made available online for self-study before course (available at least 8 weeks ahead of course)
-on day of course: very brief lectures with live demonstration reviewing contents from pre-course lectures
-Sono-social the first night of the course with dinner and live music!
Along with our talented local faculty, guest faculty this year include Drs:
Paul Mayo (Northwell University, NYC)
Bret Nelson (Icahn School of Medicine at Mount Sinai, NYC)
Seth Koenig (Northwell University NYC)
Vicki Noble (Harvard University, Boston)
Scott Millington (University of Ottawa)
Brian Buchanan (University of Alberta)
Aws Alherbish (University of Alberta)
To register and for more details please go to this link: http://www.cvent.com/d/9fq0hg
The brochure for the course can be found here
Contact [email protected] with any questions.
]]>
