Advanced critical care echocardiography case review by Hassan Raza M.D.
Suggested material to watch before this: https://www.youtube.com/watch?v=UrQKyURqDBI
Cited in the video:
SHOCK trial: https://doi.org/10.1016/s0002-9343(00)00310-7
Contemporary Management of Cardiogenic Shock: https://doi.org/10.1161/cir.0000000000000525
Tamponade, IVC vs. Aorta, and UFO!
In this episode, we discuss a rule out test for cardiac tamponade using IVC distensibility, compare the IVC to the aorta, and discuss a strange new finding that we named the Lava Lamp sign!
Tune in to listen to the discussion between Dr Robert Arntfield, Dr Marc-André Blier, Dr Bader Alshehry, and Dr Mathilde Gaudreau-Simard.
For questions, comments or feedback, please email us at [email protected]
Post-production by Hubert Gaudreau-Simard
Multimedia support by Brian Park, Meds 2023
Music: Nightchaser by Shane Ivers – https://www.silvermansound.com
Clips
Clip 1: Tamponade and the IVC; a good rule-out test.
Clip 2: IVC or aorta?
Clip 3: UFO: the lava lamp sign!
Role of POCUS DVT studies in different specialties, humbling moment in POCUS, renal TEE!
We have another great episode for you guys! Today we discuss the role of DVT studies in different medical specialties. We then move on to discuss a humbling moment in point-of-care echocardiography which highlights the different roles of POCUS on the one hand and comprehensive cardiac echocardiography on the other. Finally, we have an innovative surprise for you, an unusual assessment of the kidney with point-of-care TEE!
Tune in to listen to the discussion between Dr Robert Arntfield, Dr Jason Lam, Dr Melanie Lemay, Dr Mathilde Gaudreau-Simard and for his last appearance on the show our outgoing CCUS fellow, Dr. Thamer Alaifan
For questions, comments or feedback, please email us at [email protected]
Post-production by Hubert Gaudreau-Simard
Multimedia support by Brian Park, Meds 2023
Music: Nightchaser by Shane Ivers – https://www.silvermansound.com
Clips
Clip 1: WesternSono Screencast on conducting a DVT study
Clip 2: Humbling moment in POCUS; can you spot the anomaly on the aortic valve?
Clip 3: Innovation in POCUS; renal assessment through TEE
Role of Point of care TEE for prosthetic valves, pleural effusion or ascites and the pulsatility index in transcranial doppler
In this episode, we start by taking you through our take on the role of point of care TEE for prosthetic valves. We then discuss a case where looking beyond the pleura was important in identifying large volume ascites causing restriction of diaphragmatic excursion. Finally we touch on transcranial doppler and the pulsatility index. Tune in to listen to the discussion between Dr Robert Arntfield, Dr. Thamer Alaifan, Dr Mathilde Gaudreau-Simard and Dr Jag Brar.
For questions, comments or feedback, please email us at [email protected]
Post-production by Hubert Gaudreau-Simard
Multimedia support by Brian Park, Meds 2023
Music: Nightchaser by Shane Ivers – https://www.silvermansound.com
Clips
Clip 1: Bioprosthetic aortic valve in deep transgastric TEE view
Clip 2: Large volume ascites rather than pleural effusion likely responsible for restrictive respiratory failure
Surprising finding in the liver, atelectasis vs pneumonia, and introducing left atrial pressure!
In this episode, we start by discussing the incidental finding of hyperechoic spots in the liver, which we conclude to represent air in the portal system in this patient in septic shock. Then, we move on to the lung with the age old debate of atelectasis vs pneumonia. Finally, we touch on a more advanced application in cardiac ultrasound that is helpful in distinguishing between hydrostatic and non-hydrostatic B-lines; E/e’ to estimate left atrial pressure (LAP).
For questions, comments or feedback, please email us at [email protected]
Post-production by Hubert Gaudreau-Simard
Multimedia support by Brian Park, Meds 2023
Music: Nightchaser by Shane Ivers – https://www.silvermansound.com
Clips
Clip 1: Hyperechoic dots in the liver representing air (apologies for the gain & depth; trainees in action!)
Clip 2: Pleural effusion with consolidation
A) More likely to represent atelectasis
B) Favored to be pneumonia
Left Atrial Pressure
Click here to see the detailed PDF!
LAP helps differentiate B-lines caused by hydrostatic pulmonary edema versus inflammatory/infectious causes of B-line.
Welcome to WesternSono’s newest project, the Ultrasound Podcast! Join us in our conversations around interesting cases and emerging topics in point of care ultrasound. To all those point of care ultrasound enthusiasts out there, tune in and pick up a few pearls!
The diaphragm, lung sliding and that stenotic mitral valve!
Our first episode takes you through the importance of the diaphragm in lung ultrasound, lung sliding pearls and the pitfalls of assessing left ventricular function in the presence of mitral valve stenosis.
Listen in to the conversation between Dr Robert Arntfield, program director of the Critical Care Ultrasound Program at Western University and his three current fellows, Dr Thamer Alaifan, Dr Bader Alshehri and Dr Mathilde Gaudreau-Simard.
For questions, comments or feedback, please email us at [email protected]
Audio editing by Hubert Gaudreau-Simard
Multimedia support by Brian Park MD Candidate 2023
Music: Nightchaser by Shane Ivers – https://www.silvermansound.com
Clips
Clip 1: Consolidated lung or stomach with food; where is that diaphragm??
Clip 2: All things lung sliding; that fake lung point where pleura and pericardium meet.
Clip 3: The hockey stick sign; careful when estimating EPSS!
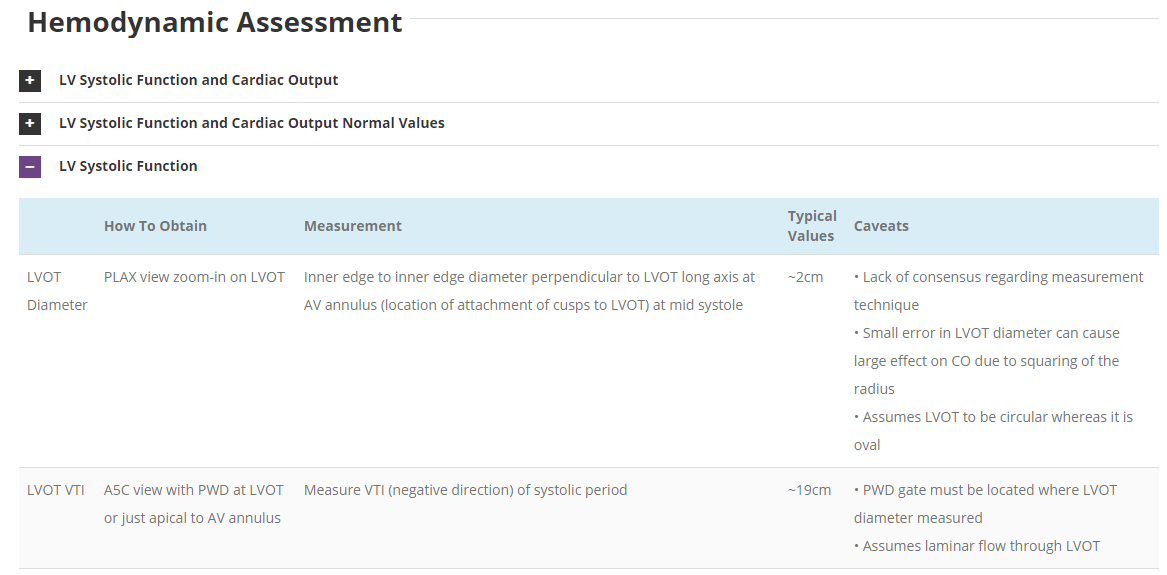
Our previous Critical Care Ultrasound Fellow, Marko Balan MD FRCPC, who is now an intensivist at Dartmouth General Hospital has put together a comprehensive, point-of-care resource containing a wealth of advanced critical care ultrasound material. You will find in it extensive coverage of quantitative techniques that can be used for the assessment of the critically ill. Topics include: hemodynamic assessment, diastology, valvular assessment, pericardial assessment, pleural assessment, transcranial doppler, and some infrequently seen lesions. Included are tips on image acquisition, interpretation values, and calculation tools. Click below to see for yourself!
The Case
This is a 58yo F with ESRD with a history of known infective endocarditis of her AV for which she had previously completed a prolonged course of IV antibiotics. She was admitted to the ICU for worsening dyspnea. The POCUS team performed cardiac exam with some of the most striking clips shown below. What do you think? What complication of her endocarditis is shown and how would you grade its severity?



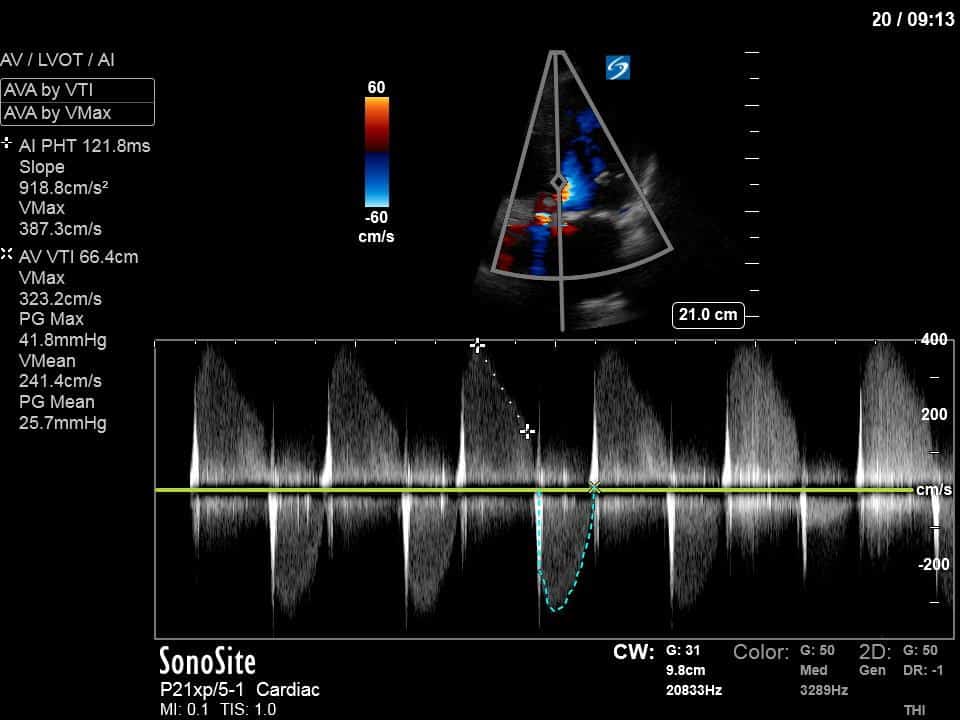
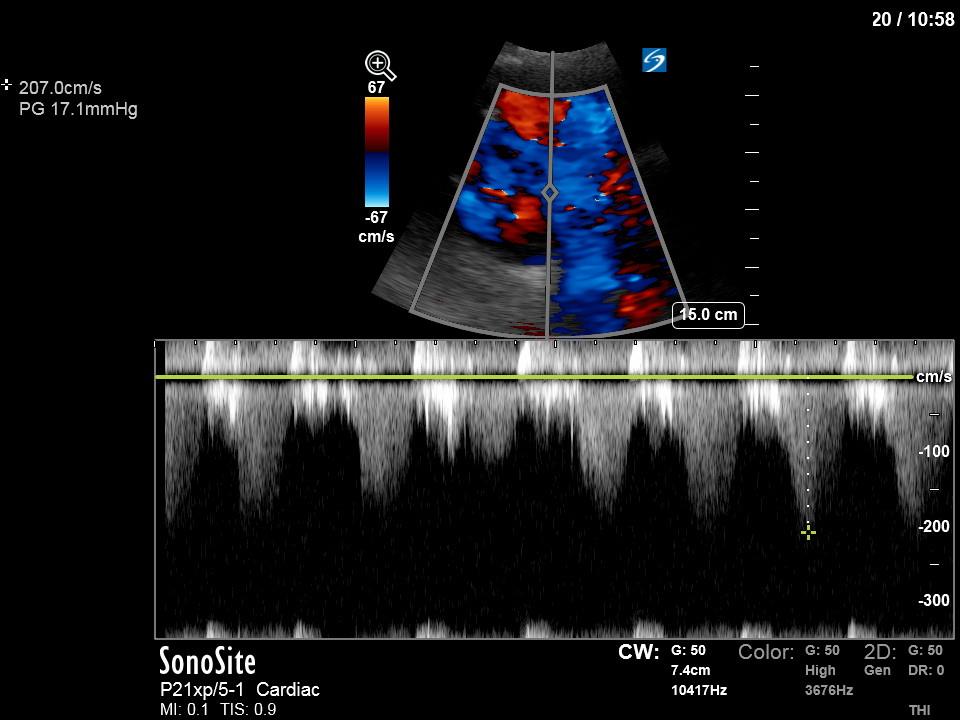
First, you can see at least a single large hyperechoic lesion primarily localized to the left coronary cusp of the aortic valve. This is consistent with her known infective endocarditis. However, now you can also see significant flail of that cusp. With just the 2D images you would expect severe aortic regurgitation (AR). It’s always a good practice to predict what the regurgitation jet will look like before putting colour doppler on the valve! Application of colour doppler then confirms an extremely large anteriorly directed AR jet.
From both the 2D morphology and function of the valve, and from the qualitative interpretation of the AR colour jet, we can appreciate that this is severe AR. One of the easier ways to then more quantitatively grade the severity is the measurement of the pressure half-time (PHT) which is demonstrated. The more rapidly the flow velocities of the AR slow the faster the pressure equalization between the aorta and the LV which is indicative of the severity of the AR. A PHT of < 200ms is consistent with severe AR, between 200-500ms moderate and > 500ms is mild. In this case the PHT of 113ms is concordant with our qualitative assessment of classifying this as severe AR. The subsequent spectral tracing also includes the flow out of the AV and shows increased velocities showing that the lesion is also causing aortic stenosis (AS). When we trace the spectral envelope, we get a Vmax of 3.2m/s, and a mean gradient of 26mmHg. This is consistent with at least moderate AS as well!
Thus, this patient developed severe AR (and moderate AS) as a complication of her infective endocarditis. This is likely the basis of her worsening dyspnea and meets indications for urgent intervention with cardiac surgery.
The Case
This was a case of an 80 yo M, previously healthy, with no known significant previous medical history. He presented to the ED with acute decreased level of consciousness. The leading concern was acute spontaneous ICH. He was intubated and taken for a CT Head which surprisingly was completely normal. He was subsequently transferred to the ICU with the diagnosis of altered LOC NYD. A POCUS study was performed, and several cardiac clips are shown below. What do you think? Does this give a potential clue to what could be going on? 
These clips show significant multivalvular pathology. The most obvious striking abnormality is the significant hyperechoic structure mostly localized on the posterior mitral valve leaflet (PMVL). Although this has a differential, this was favoured to be severe mitral annular calcification (MAC). Given the size and significance of the MAC there was further concern that this may be have provided substrate for an embolic basilar artery stroke as the cause of his decreased LOC. He was taken back for an immediate CTA which again was normal. However, the next day, an MRI was performed which unfortunately showed catastrophic multifocal, bilateral infarcts involving cortical, subcortical and brainstem structures consistent with an extensive cardioembolic etiology. Although this was an unfortunate outcome, this case still captures the power of POCUS to shed light on what was very much an undifferentiated patient with altered mental status. The study prompted further consideration of a cardioembolic stroke and expeditated the necessary investigations. Furthermore, hemodynamically significant valvular lesions (see below) were also recognized which allowed the team the alter their management to keep the patient stable while further investigations were completed.
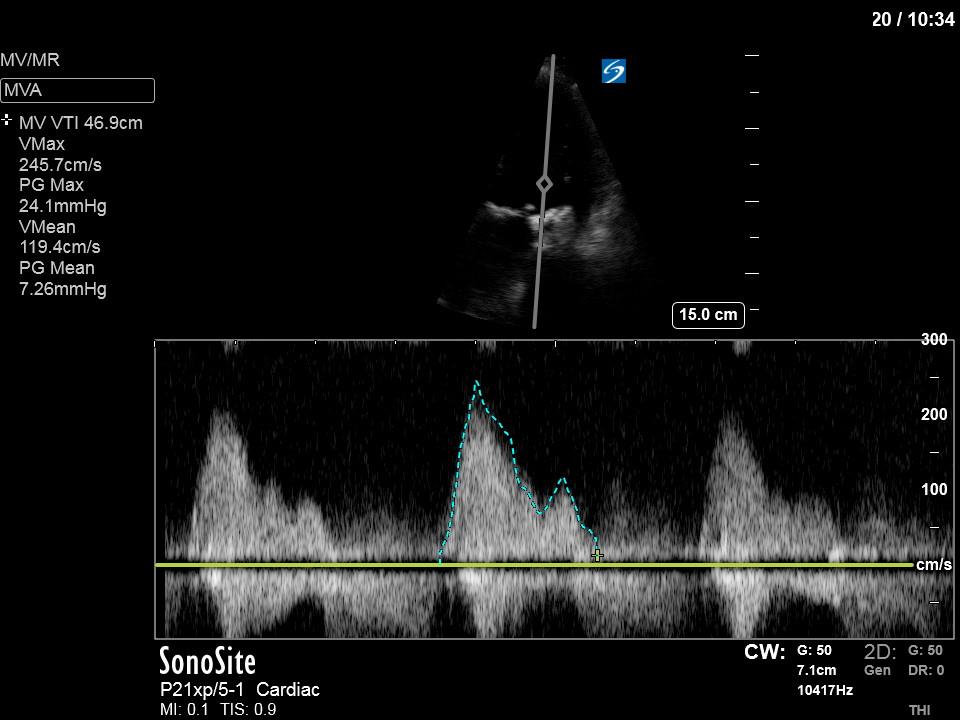
As a result of the PMVL pathology there is at least moderate mitral regurgitation which is only partially captured in the above clips. Furthermore, you can also notice flow acceleration through the MV suggestive of mitral stenosis. Interrogation with CW (PW was aliased in this case) shows the very high (~2m/s) mitral inflow E-wave velocities. We can then trace the mitral inflow to get a mean gradient which in this case was approximately 7 indicating moderate mitral stenosis.
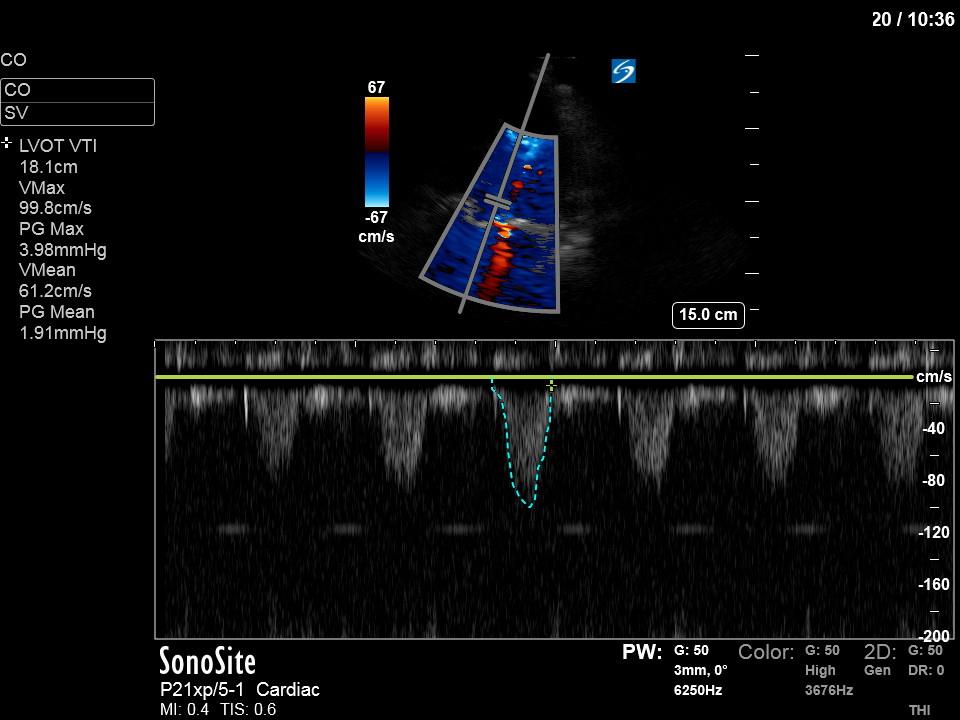
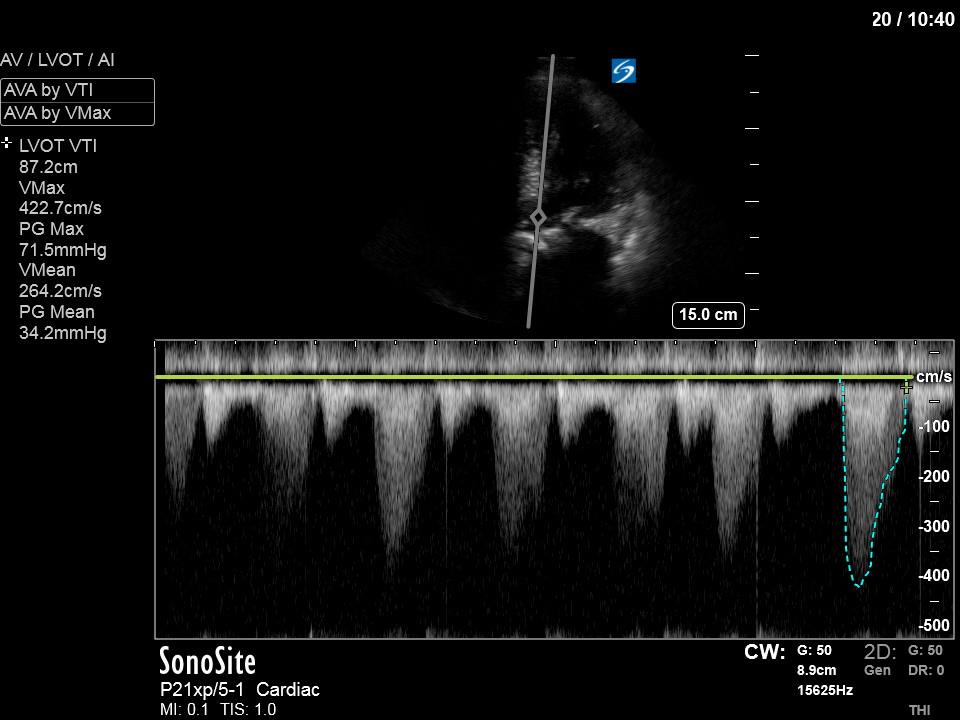
The aortic valve is also heavily calcified with very limited opening highly suggestive of significant stenosis. Thus, this was also interrogated with Doppler to further quantify its severity. First, PW Doppler was used to measure the LVOT VTI which was around 18cm. Next, CW was placed through the AV, which when traced, gave an AV VTI of 87cm, a peak velocity of 4.2m/s, and a mean gradient of 34mmHg. The dimensionless index (LVOT VTI/AV VTI) was therefore 0.21. Although the mean gradient of 34mmHg is in the moderate category the rest of the parameters converge on this being severe AS. Thus, POCUS was able to quickly discover severe multivalvular pathology that was not previously documented.
This case again highlights how the deployment of POCUS can uncover significant pathology which can dramatically alter the hemodynamic management of patients, and simultaneously aid in determining the ultimate diagnosis of the patient.
Thanks for reading!
Matt
The Case
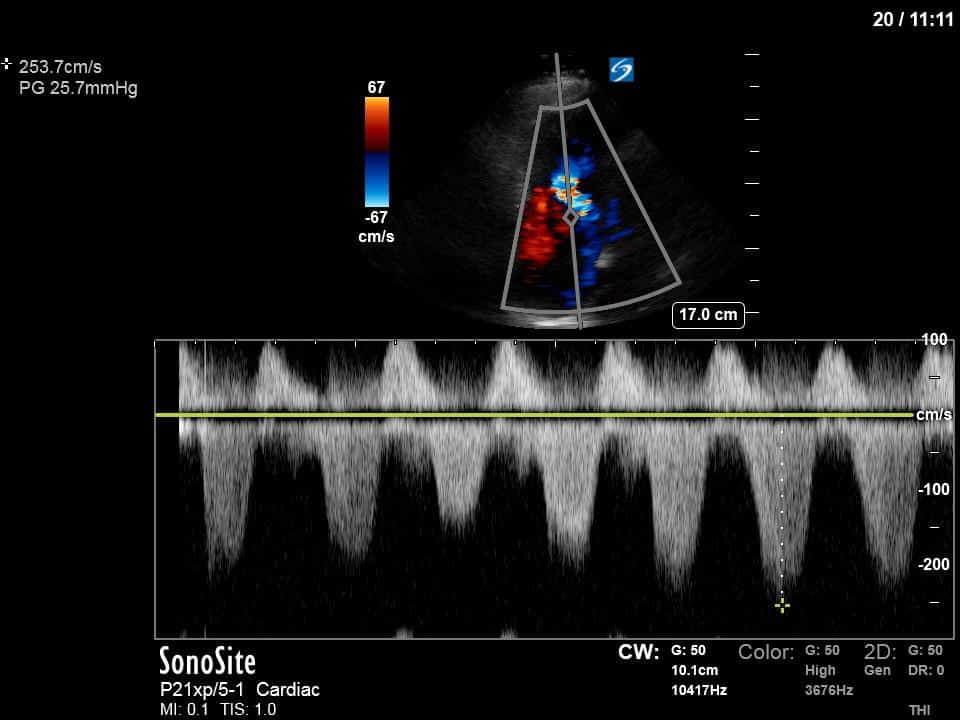
This is 65 yo M who presented with acute hypotension, hypoxia, and worsening AKI in the setting of known severe pulmonary hypertension secondary to a previous PE (CTEPH). He was admitted to the ICU for consideration of CRRT and IV flolan. A few days into his admission, the team asked for a POCUS cardiac assessment to reassess the status of his RV. Have a look the images below. Specifically, what do you think about the tricuspid regurgitation and estimated RVSP?
This is an example of severe RV dilation (and RA) and dysfunction. The RV is completely overriding the LV on the apical 4-chamber and in the parasternal short axis you can appreciate the D-shaped septum during both systole and diastole suggestive of both pressure and volume overload.
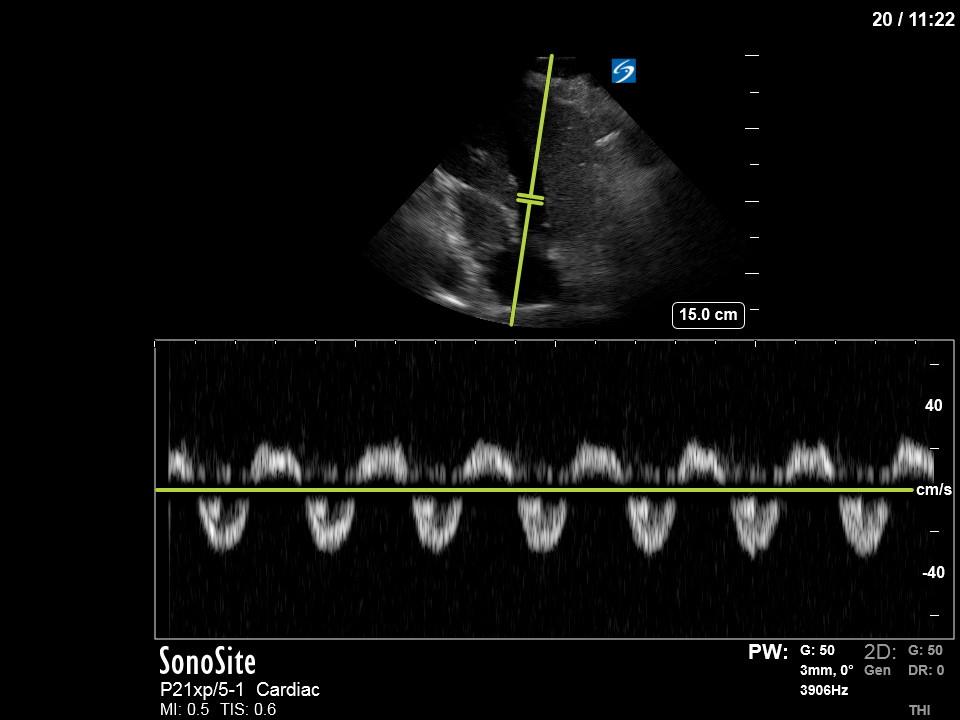
The TR has been interrogated from both the RV inflow window and the A4C window. You can see a large, severe appearing jet, directed towards the septal TR leaflet. There are a variety of parameters that can be used to quantify TR, however, there are several immediate features that suggest this is severe TR without having to resort to some of these more advanced methods. First, using a qualitative analysis of the continuous wave (CW) spectral doppler tracing (from both the RV inflow and A4C windows) shows a highly dense, and at times quite triangular signal. These aspects are both consistent with severe TR. More mild forms of TR are usually less dense and more parabolic in shape. Furthermore, pulse-wave (PW) doppler of the hepatic vein shows systolic reversal of flow which is also suggestive of severe TR.
In this case the importance of recognizing that this is severe TR is that in this setting, the usual way of estimating RVSP can’t be relied upon. Usually, we apply the modified Bernoulli equation () to get the pressure gradient between the RV and RA and then add on the estimated RAP. However, in the setting of severe TR, the right atrial pressure (RAP) will increase rapidly during systole which will result in an underestimation of the RVSP. This is likely the case here as the highest-pressure gradient was only 26. There are also some other, more physics-based reasons, why in the setting of severe TR the simplifications implied in Bernoulli equation itself may break down contributing its inaccuracy.
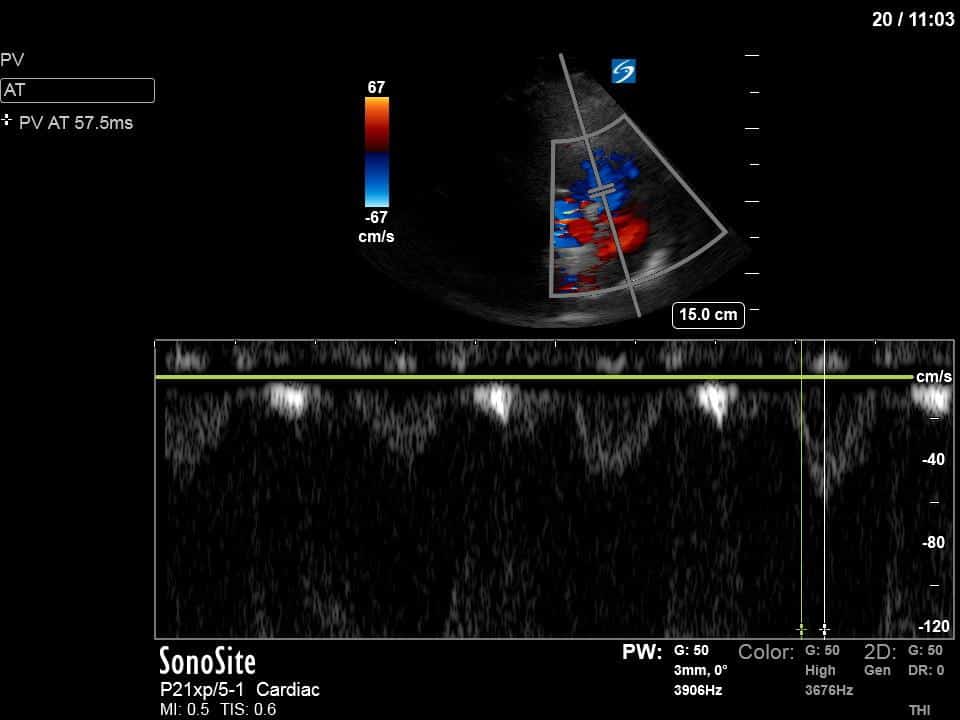
We also interrogated the RVOT with pulse-wave doppler and measured the pulmonary artery acceleration time (PAT). Using this we can also get an estimate of the mean pulmonary artery pressure (mPAP). There are a variety of formulas but a simple one to remember is mPAP = 80 – 0.5(PAT). In this case, the PAT of 57 would yield a mPAP of ~52mmHg. This value is more in keeping with his known severe CTEPH.
Although estimating the RVSP is a great way to quantify the severity of RV pressure overload this case illustrates a potential pitfall of this method and highlights another Doppler technique that can be deployed for this purpose.