The Case
This is a 40-year old man status post-liver transplant (several months prior) who has had a complicated hospital course. He is now re-admitted with presumed septic shock (query HAP) and has been intubated for respiratory failure. He’s also had a formal abdominal ultrasound commenting on periportal hepatic edema and signs of congestion.
Based on the images below what interventions might you make to the team in addition to antimicrobial therapy? The team is particularly worried about right heart failure and elevated right-sided pressures – what do you tell them based on your findings?
Here with have a cardiac study with a few abnormalities. The most striking in the initial clips is the RV – it is markedly dilated (almost bigger than the LV; a normal RV should be less than 2/3 the size of the LV) and has impaired systolic function. Visually, we can see reduced vertical movement of the lateral tricuspid annulus and reduced free wall excursion.
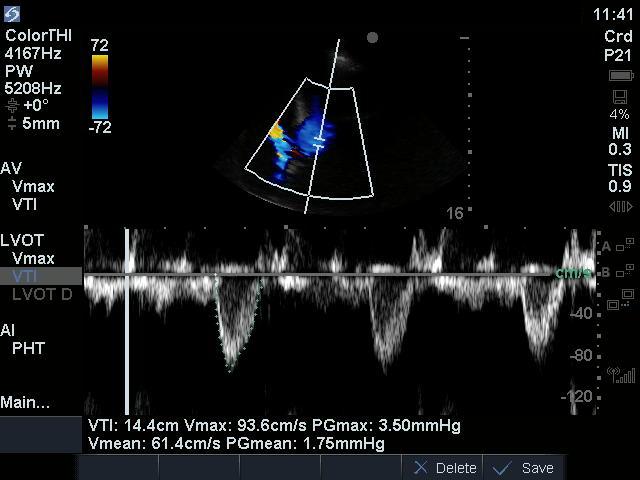
The left heart also appears to have mildly impaired function, which was previously. In measuring the LVOT VTI, we see that it is reduced at 14.4 (normal is 18-22) – this likely reflects a combination of mildly reduced LV contractility, as well as poor delivery of blood to the LV due to an impaired RV.
To answer our first question, then – the POCUS team suggested diuresis (to offload the struggling, dilated RV) and consideration of inotropy. Fluids, often a reflex response in cases of suspected sepsis, would not have done this patient any favours as they simply would have worsened the right-sided overload.
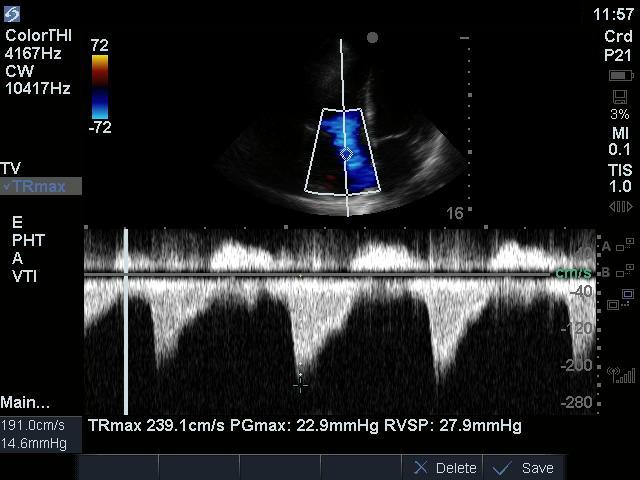
Next, to address the second question – is there elevated right-sided pressure? We’re highly suspicious based on the 2D images of the RV, but we need more information. Interrogation of the tricuspid valve with colour doppler reveals severe tricuspid regurgitation – there is a large aliased jet that easily hits the back wall of the RA. We can use the TR jet to calculate RV systolic pressure (RVSP), as RVSP = (TR jet max PG) + (estimated RAP). For more on this and a review of Doppler basics, see this screencast: https://westernsono.ca/principles-of-doppler/.
We can see, then, that when we interrogate the TR jet with CW, we obtain a TR maximal pressure gradient. Surprisingly, however, despite other signs of right-sided overload in this study, our measured PG is a measly 23. What’s going on here?
Both the colour doppler clip and the CW tracing provide clues. The key here is the severity of the TR – which is observed both visually with a large, high-velocity jet, as well as in the CW tracing. Note the density of the velocity waveform tracing – it appears just as bright and dense as the blood above the baseline, suggesting that just as much blood is flowing backwards through the tricuspid valve as is flowing forwards into the RV.
In the presence of very severe TR, our calculated TR pressure gradient can underestimate RVSP. This is because of the rapidity of the equalization of pressures between chambers – that is, there is such a large regurgitant lesion that the RA and RV pressures equalize very quickly, before a large pressure gradient can develop.
Our team interpreted these findings in context and confirmed the likely presence of elevated right-sided pressures to the treating physicians, although we could not measure them using this method. After diuresis and extubation – both of which are RV-friendly interventions – the image below demonstrates a noticeable improvement in RV size and function.
That’s all for this week. Thanks for reading folks, and happy scanning!





