A blithesome beginning of the week my B-line chasing brethren (and sisteren?)
Hopefully you’ve all returned home energized from the recent CRUS course and are ready to Make Artefacts Great Again! If you’re still looking for a little extra inspiration, the COTW/COTG has you covered, so let’s get down to business.
The Case
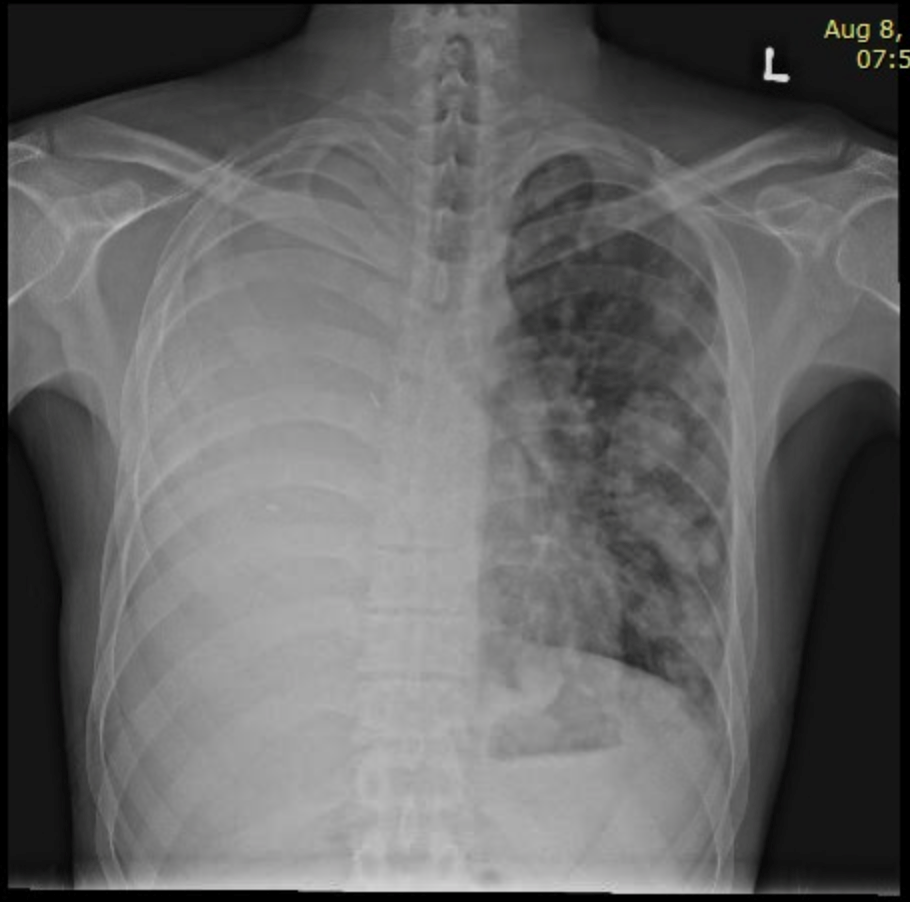
Our first case features a 69F admitted with SOB and general unwell which persisted after initial left thoracentesis for anticoagulation associated spontaneous hemothorax. What do you see, or should I say see(s).
COTG
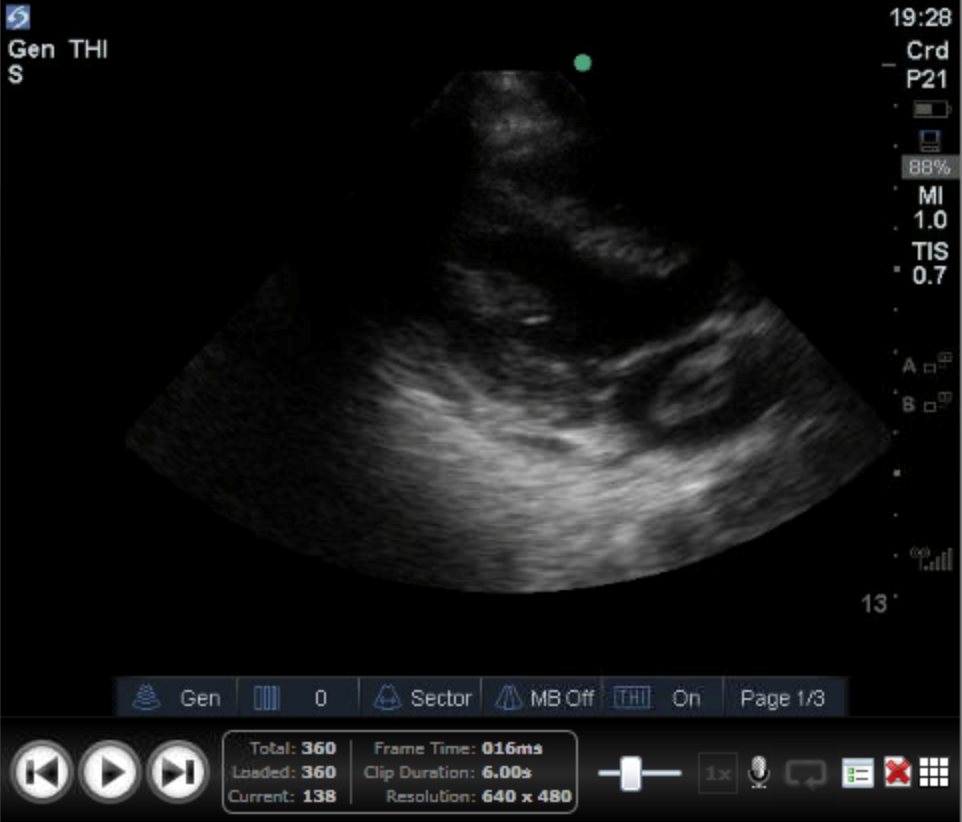
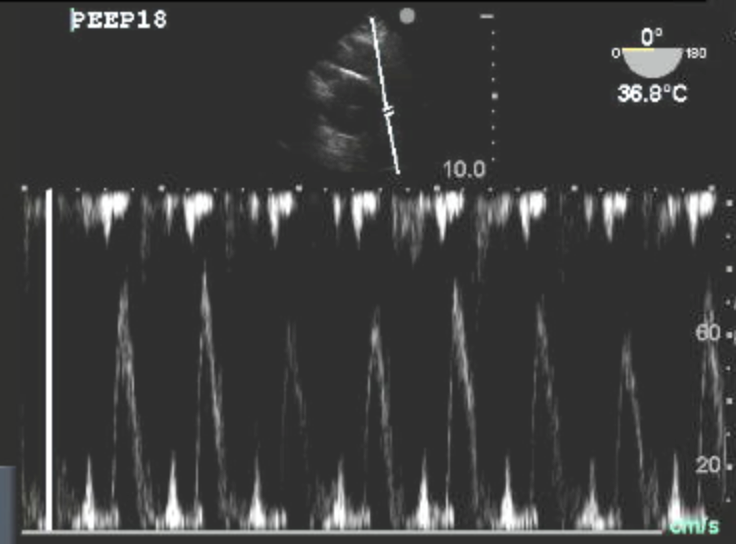
Our COTG comes to us from an 82M who’s being transferred for AKI in setting of recent large ischemic stroke. Any takers on possible aetiologies? What would you look for next? Also, no he isn’t suffering from myxedema coma, the clip has just been slowed down for your viewing pleasure.
Answer to Last Weeks Case
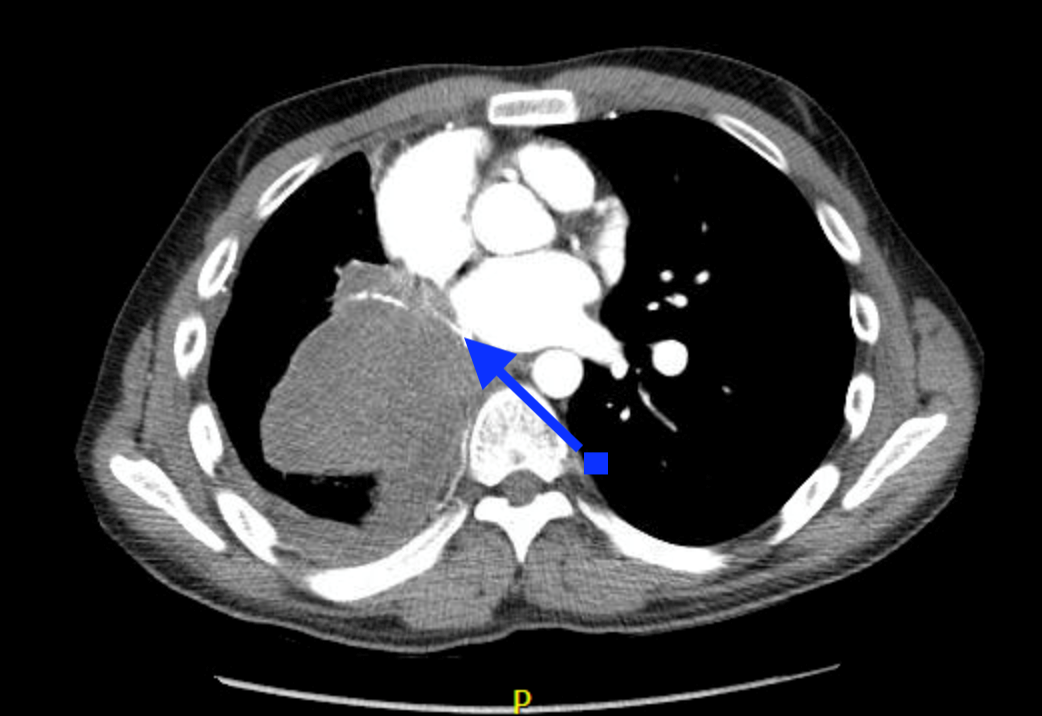
Well that shouldn’t be there… The clip from this young gentleman showed a large mass with an independent motion that was in the left atrium during systole and plopped (see I haven’t forgotten you stethoscopy enthusiasts) into the left ventricle during diastole. Differential diagnostic considerations would include endocarditis, clot in transit (particularly paradoxical embolism), ruptured papillary muscle and tumour. Beam thickness artefact is a frequent mimicker of mass in the left atrium or ventricle but should lack an independent movement as seen here. In this unfortunate young man’s case, this is like metastases from his testicular primary which were initially in the left lower lobe but have likely eroded through the pulmonary veins into is left atrium. On another unfortunate note (although admittedly not at all on the same scale), someone told me this patient must’ve had a great tumour plop on auscultation and I died a little inside. … ….. Any-who, if you’re interested in learning more on how to evaluate cardiac masses, check out the article (The echocardiographic evaluation of intracardiac masses a review.)

Answer to Last Weeks COTG
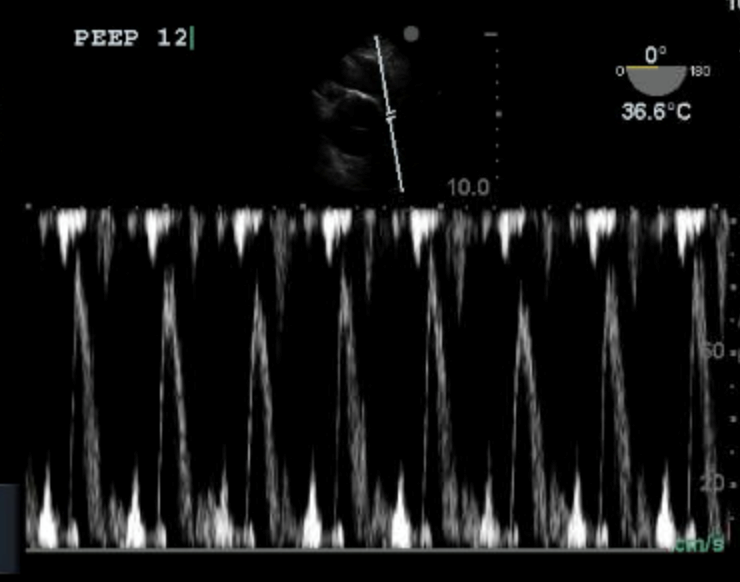
Hello pulmonary artery my old friend
I’ve come to pulse-wave doppler through you again
Inspiratory variation suggests an RV failing
All that PEEP has got it ailing
Overdistension of the lung is the intensivist’s bane
Optimized compliance we shall attain
with the aid of echo.
For all you guys who don’t know this Simon & Garfunkel classic (or the great Disturbed cover), you’re missing out. Also, to get back on topic, the PW image through the Pulmonary Artery shows that there is a hefty respiratory variation in PA VTI (and so RV cardiac output). This suggests that tidal ventilation is increasing RV after load (through increased pulmonary vascular resistance) which is related to over distension of regions of lung with alveolar pressure surpassing capillary pressure. This is undesirable. The PEEP was dialled down until we were left with this PW trace, showing much less variability. The POC TEE wizards in France led by Antoine Vieillard-Baron showed titrating PEEP to minimize RV stroke volume variation correlated with optimizing quasi-static compliance (see attached article). And in the era of minimizing driving pressure, that’s something everyone can enjoy. Fair warning, optimized compliance may not equate to optimized oxygenation (you may have to increase FiO2 a little, but you will be able to decrease driving pressure). If you don’t have access to TEE, the pulmonary artery can also be found on the PSAX or SXSAX at the aortic valve/RV inflow-outflow view and the same evaluation can be made (although the pictures may not be as pretty). PEEP TITRATION PAPER