Hello POCUS enthusiasts!
Amanda Young, PGY5 in critical care, here. I decided to dip my toes into the POCUS QA waters and take on a more senior POCUS role this past week. We had some great cases this week, and I thoroughly enjoyed myself, so I hope you enjoy the cases we’ve singled out.
The Case of the Week is brought to us by Dr. Ahmad Alenazy, a visiting critical care fellow from McMaster University. The Case of the Geek is brought to us by Dr. Darren Weaver, GIM fellow. Let’s get straight into it!
The Case
A 47 year-old female is admitted to ICU for respiratory failure and sepsis. She has a history of immune suppression and has had a prolonged stay in ICU. She is requiring pressors and the POCUS team was asked to assess cardiac function. Here are some of her echo images:
COTG
A 60 year-old male with a history of cirrhosis is admitted to ICU with an upper GI bleed requiring insertion of a Blakemore tube. His hemodynamics stabilize, and the POCUS team was asked to assess for volume overload. Here are some of his echo images:
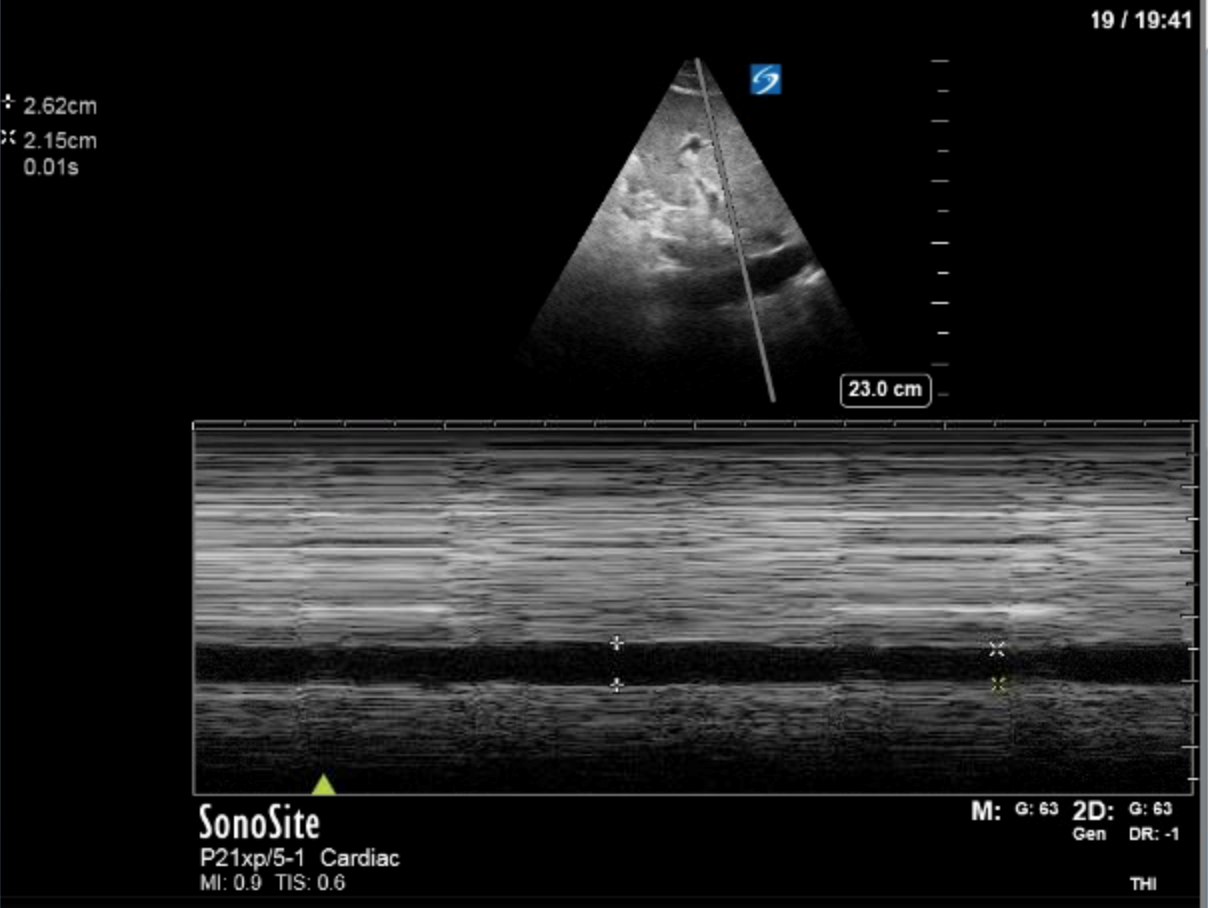
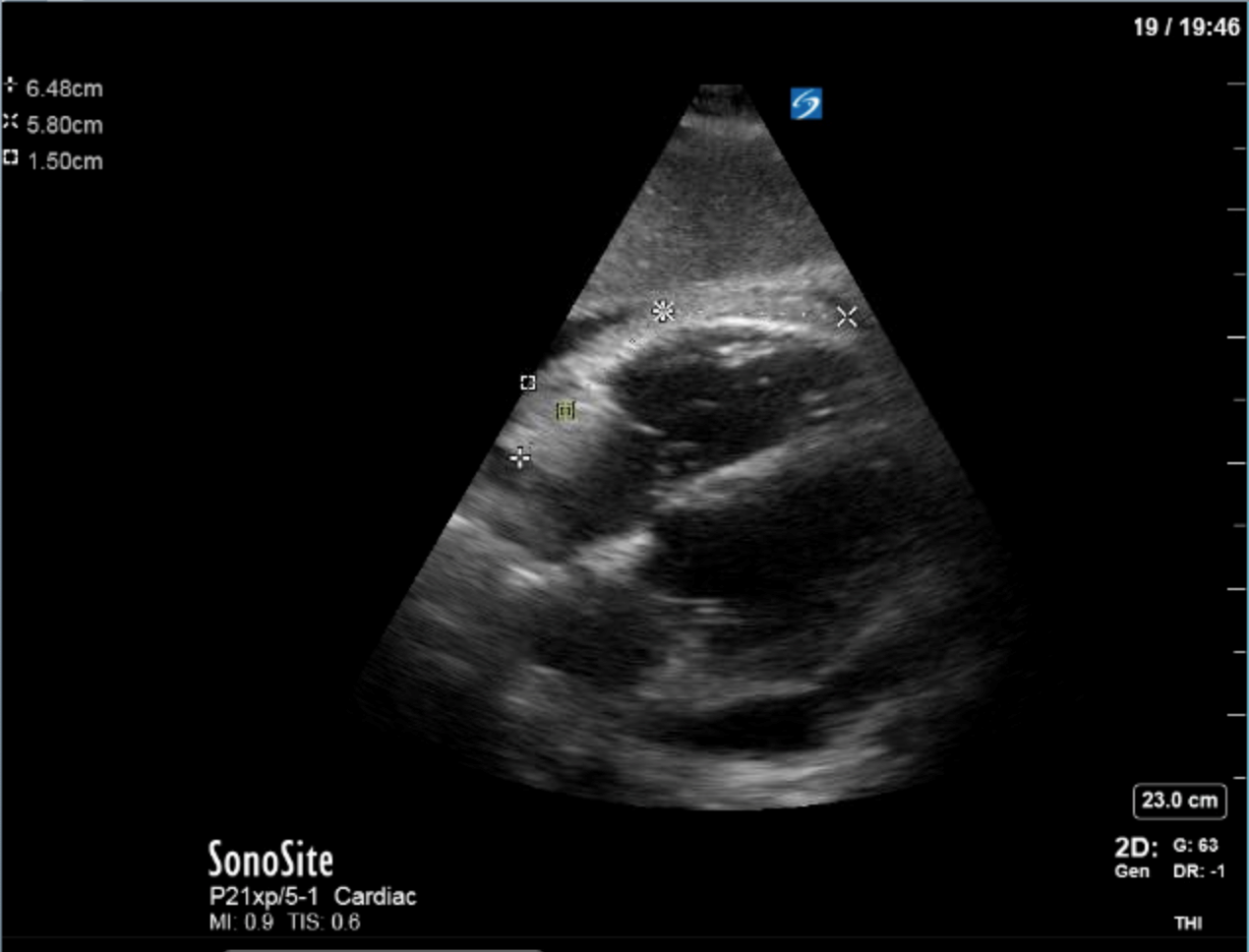
1) This patient has a moderate pericardial effusion. Pericardial effusions are classified as small if they are <1 cm, moderate if they are 1-2 cm, and large if they are >2 cm. This can be measured at end diastole along the posterior wall of the LV.
The question now is: to tap or not to tap?
In this case we would not recommend pericardiocentesis at this time for the following reasons:
- We do not observe RA collapse during ventricular systole (i.e. when the RA should be filled). RA collapse for more than 1/3 of the cardiac cycle is almost 100% sensitive and specific for cardiac tamponade, and this is not seen in this patient.
- We also do not observe RV collapse during ventricular diastole in this patient. In early tamponade this will only be present during expiration (in a spontaneously breathing patient), but as intrapericardial pressures increase this may be present in inspiration as well. This sign is more sensitive and specific for cardiac tamponade than our trusty pulsus paradoxus measurement at the bedside.
- *NB: the above signs may not be present in patients with pulmonary hypertension, positive pressure ventilation or severe LV failure.
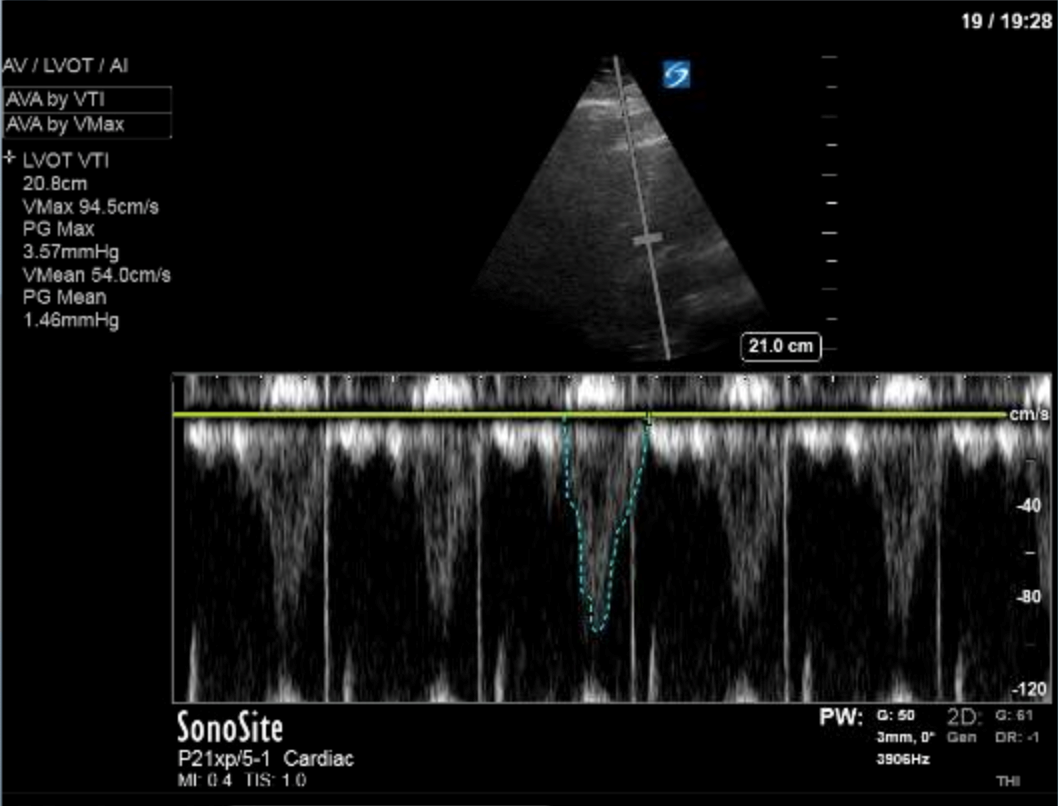
- This patient has a normal cardiac output as shown by the VTI measurement. With significant tamponade we should see reduced cardiac output.
- *NB: this patient does have a mildly dilated IVC (>2 cm), which is sensitive for cardiac tamponade. However, it is a non-specific finding, and should not be used as the sole determinant for tamponade. If they do not have a dilated IVC then it’s very unlikely that they have cardiac tamponade and you can rule it out, but if they do have a dilated IVC it does not mean you can rule in cardiac tamponade. You should look for other signs of tamponade.
Reference: Perez-Casares, et. al. Front Pediatr. 2017; 5: 79.
2) This patient has a prominent epicardial fat pad over his RA and RV. It is the isoechoic density that is well-seen over his RA and RV.
A and B are incorrect as we do not see features of these pathologies on these images, and D is incorrect as we see the RA is well filled during ventricular systole (also known as atrial diastole).
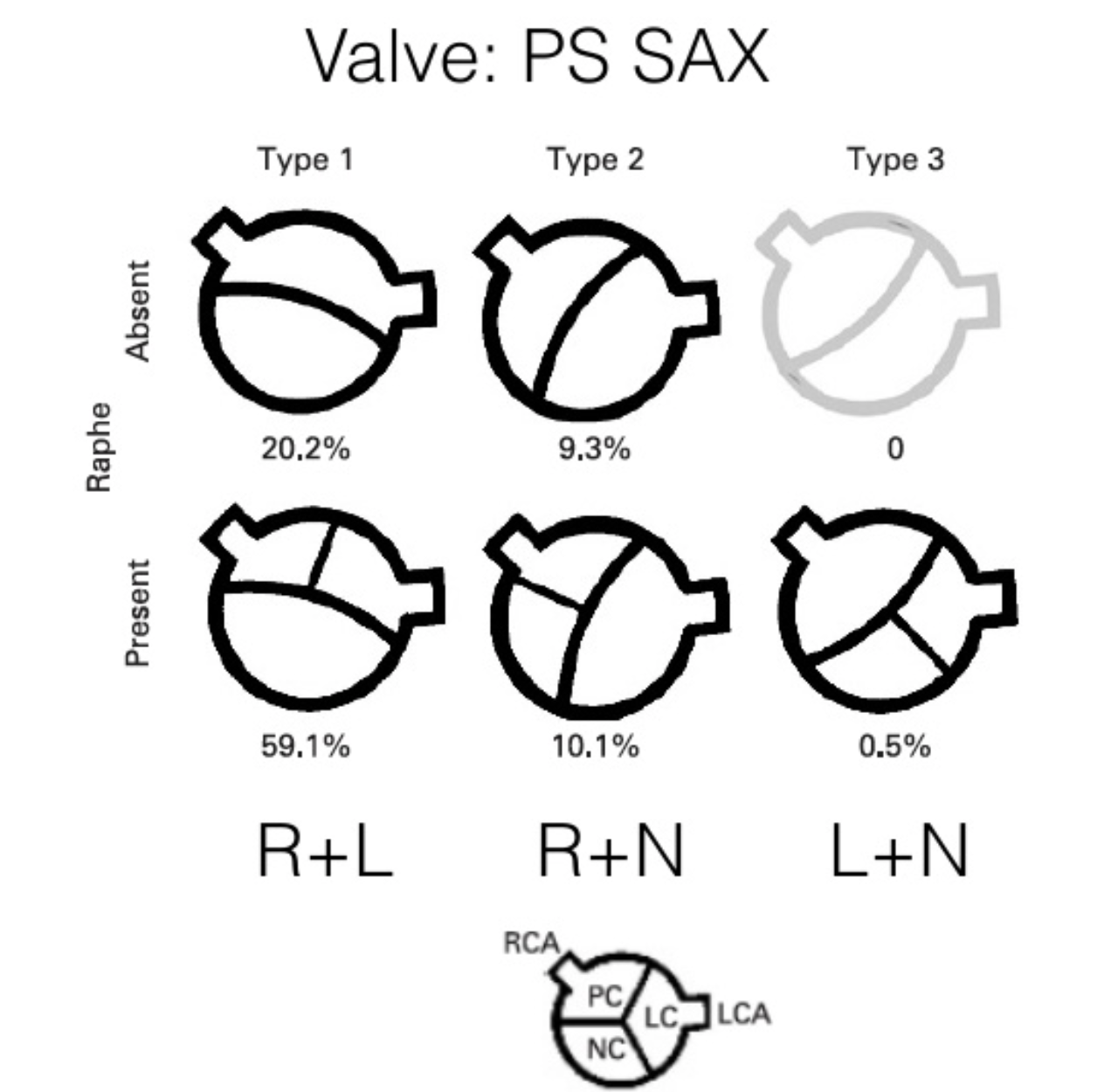
1) This patient has a bicuspid aortic valve (BAV). Bicuspid aortic valves are present in approximately 0.5-2% of the general population (M:F 3:1) and are associated with earlier onset aortic stenosis and aortic regurgitation secondary to aortic root dilatation, valve prolapse, and endocarditis. In TTE, sensitivity and specificity for identification of BAVs are 92% and 96%, respectively. Features of a BAV in TTE include systolic doming, which is seen in the parasternal long axis view in this patient, and a raphe which is often better seen in the parasternal short axis view with the probe tilted towards the patient’s right shoulder in order to view the AV in an axial plane. Bicuspid aortic valves can be classified by their appearance on TTE in this view. Our patient appears to have a type 1 BAV with raphe present.
Here, A and C were incorrect as there was no evidence of a vegetation in these images. D was also incorrect as there was no evidence of RV dilation in these images. More views of the RV would be ideal, but our 1:1:1 RVOT:LVOT:LA ratio was preserved here.
References:
- Ayad et al. Am J Cardiol 2011; 108:1589
- Schaffers et al Heart 2008;94:1634–1638
2) There is no severe AR in these images. There is no well-defined AR jet here. The colour we are seeing coming into the LV during diastole is likely blood flow into the LV from the LA.





