Hi POCUS people,
I hope you all enjoyed a lovely Remembrance Day weekend. Here in London we got our first sprinkling of snow, which was highly exciting for this Vancouverite. Bring on the holiday season!
The Case
This case comes to us from Dr Heather Hames from our fantastic ED POCUS contingent. This was an elderly gentleman who presented with weakness, falls, and cachexia (no abdominal pain, remarkably). POCUS was shocking – what’s going on in these clips?? (First is right flank, second is left flank, third is midline/peri-umbilical).
COTG
These are 2 images from a 64-year old gentleman who suffered a significant subarachnoid hemorrhage. What are we looking at on this scan, and what conclusions can we draw based on our findings?
Eye Scandy
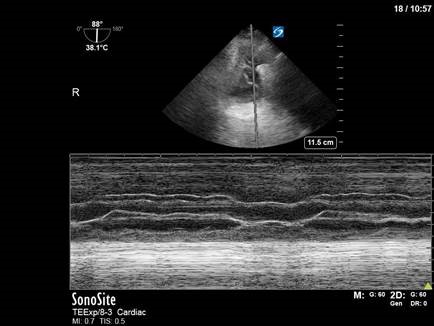
Perhaps a bit morbid for #eyescandy, but a super cool scan nonetheless. This is a TEE clip taken from an intra-arrest study, demonstrating rapid clot formation in a heart in cardiac standstill. Clinically, this was helpful for guiding termination of resuscitation.
Answer to Last Weeks Case
This is an interesting clip in an apical 4-chamber view of the heart. The right ventricle looks reasonable; the left ventricle has reduced contractility, particularly the septum and apex. But the most striking thing about the image, of course, is the echogenic density seen in the middle of the LV, which seems to be crossing the mitral valve into the left atrium. What’s going on here? Is this a huge clot? Tumour? Some horrific complication from her CABG (those damn surgeons)?
If you said d) none of the above, you’re correct. This is an excellent example of ultrasound artifact that can, at first, look very sinister. There are a couple key clues that can help us identify this as artifact: the echodensity does not move with contraction of the heart (contrary to tumour or thrombus), it does not seem attached the the myocardium, and it crosses in an unusual fashion from the LV to the LA. Furthermore – and this is the kicker – it is not visible in other views, such as a parasternal long or short-axis view.
Ultrasound artifacts are generated due to characteristics of the ultrasound beam itself, the presence of multiple echo beams, or errors in velocity or attenuation. Understanding how artifacts are generated, and learning how to recognize them, is key to generating and interpreting reliable POCUS images, as they can sometimes be very tricky! The attached paper provides a nice review of the various types of ultrasound artifacts.
Answer to Last Weeks COTG
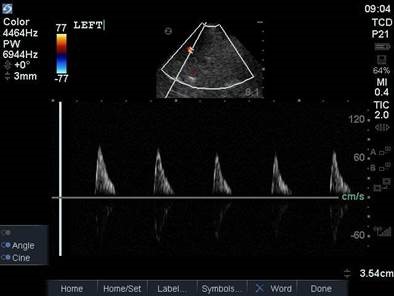
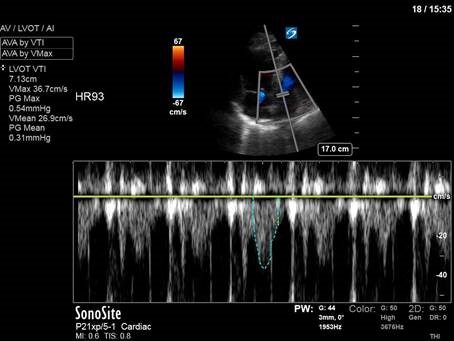
Another fantastic TEE case this week. It’s hard to tell from the small screenshot, but here we’re in a modified RV inflow/outflow view in the mid/upper esophagus, with the pulmonary artery screen right and aligned parallel to the ultrasound beam. (A view with vertical alignment of the PA can be tricky to find in some patients, and may be best seen from different axes – it can be a case of trial and error). In this patient, this view allowed us to place a pulse-wave doppler over the pulmonary artery and obtain a VTI of the RV outflow.
In the first image, at a PEEP (positive end-expiratory pressure) of 20 cmH2O, you can appreciate a decrease in the height of the VTI tracing during inspiration. This is a visual representation of a negative heart-lung interaction: in this case, higher levels of PEEP are making a compromised right heart work against a high afterload, and are causing reduced RV output during inspiration. In contrast, in the second image with PEEP reduced to 10, we see no variation in RV outflow VTIs with inspiration – indicating that there is no negative effect of the ventilator being exerted on the right heart. Here we have just eyeballed the measurements to look for visible variation with respiration, though some groups advocate measuring the VTIs to obtain a more quantitative assessment.
PEEP titration and optimal ventilation strategies is obviously a complex topic beyond the scope of this e-mail. The attached paper by Schmitt et al provides more detail on the technique of PEEP titration using RV doppler measurements by TEE, for those interested.
For our patient, his PEEP re-set to the lower value of 10 cmH2O. This decision was supported by lung ultrasound findings using TELUS (trans-esophageal lung ultrasound) that showed largely aerated lungs, indicating that high PEEP for lung recruitment was unnecessary. He did well with the lower PEEP setting, with an improvement in hemodynamics and no change in his oxygenation.
That’s all for this week folks. Happy scanning!
The POCUS Team





