Hi everyone,
Thought we would take a break from the world of echo this week and again illustrate how we are using transcranial doppler in the ICU at Western.
The Case
This is a case of a 52 yo F trauma patient with severe traumatic brain injury. She was intubated and transferred to the ICU where, given the severity of her TBI, an intraparenchymal ICP monitor was placed by neurosurgery. The ICP monitor was initially showing an ICP of 10. Overnight, however, despite no apparent clinical change, the ICP waveform was inconsistent and the readings were now showing values around 40-50. We thus performed a point-of-care TCD to help determine whether her ICP was truly elevated or whether the ICP monitor was giving spurious information. Have a look at the following images. Do you think the TCD spectral waveform is consistent with markedly elevated ICP?
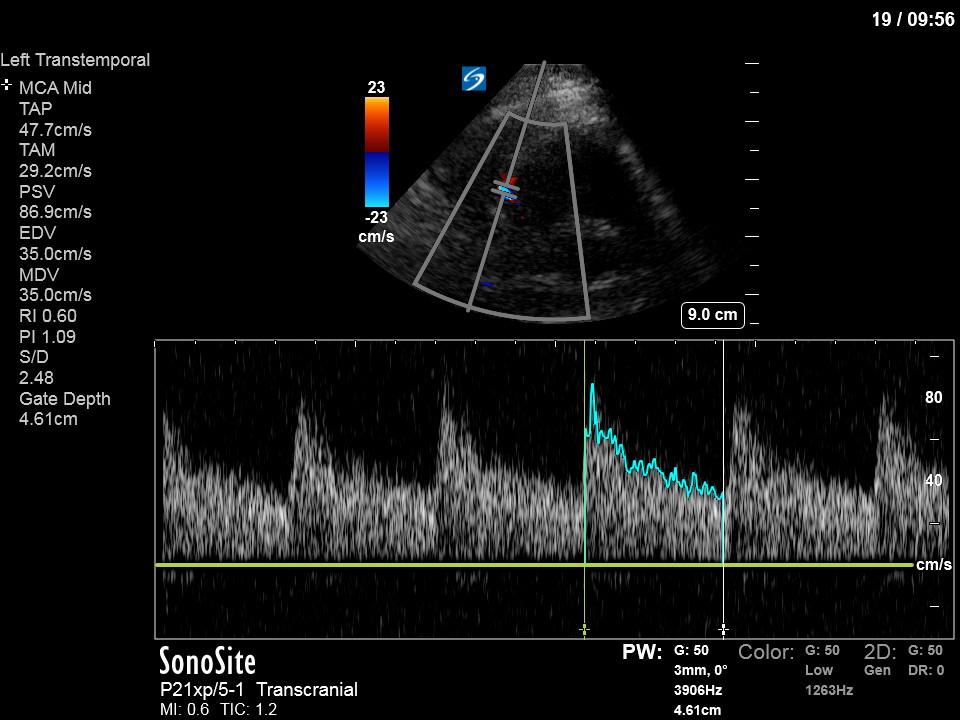
The above images show pulse wave doppler interrogation of the left MCA artery. This produced the typical spectral Doppler velocity waveform with a steep systolic upstroke and the gradual step-down diastolic flow. This is the expected appearance of flow in the absence of raised intracranial pressure.
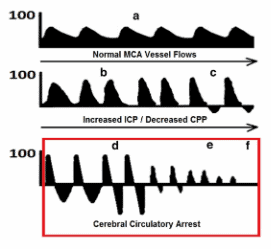
In the setting of raised ICP the diastolic flow becomes blunted, and can even progress to diastolic flow reversal followed by the gradual reduction of systolic flow as the ICP progressively increases towards cerebral circulatory arrest (see Figure below from Lau’s paper attached below).
Pulsatility index (PI) = (Peak systolic velocity – End diastolic velocity) / (Mean velocity)
From the PI (which machines with the TCD software package will give you automatically from tracing the spectral waveform) you can get the ICP through the following formula:
ICP = (10.93 x PI) – 1.28
In this case the PI was found to be 1.09. Therefore, using the above formula:
ICP = (10.93 x 1.09) – 1.28
=10.6 – essentially a normal ICP
Given the normal waveform and estimated ICP the parenchymal ICP monitor was thought to be non-functional. Neurosurgery was re-consulted and the ICP monitor was exchanged for an external ventricular drain (EVD) which showed a normal ICP of 10, corroborating our TCD results.
This case illustrates the utility of point-of-care TCD to help guide the management of the neurocritical care patient. See the attached article below by Lau & Arntfield detailing the use of point-of-care TCD by intensivists.
Click here: TCD





