Hi fellow Ultra-geeks,
The POCUS team at here Western had another great week full of interesting clinical cases and long, in-depth discussions about pleural morphology, diastology, and the meaning of life. The usual.
The Case
This case comes from our ED POCUS friends, and adds some very welcome variety to the abundance of heart and lung scans we’ve seen in the past few weeks.
This was a middle-aged woman presenting with abdominal pain, which has now somewhat settled. Her labs are normal. Can we pinpoint the cause of her pain from this scan?
COTG
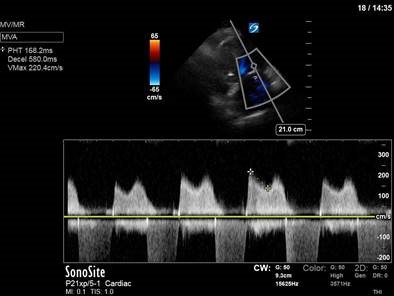
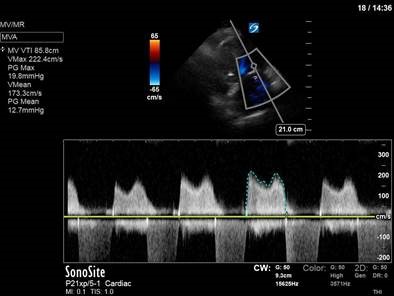
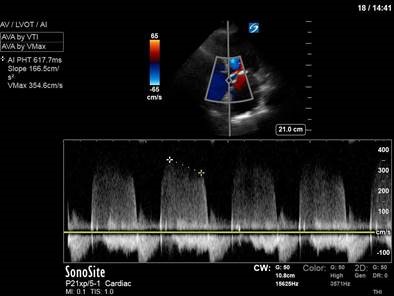
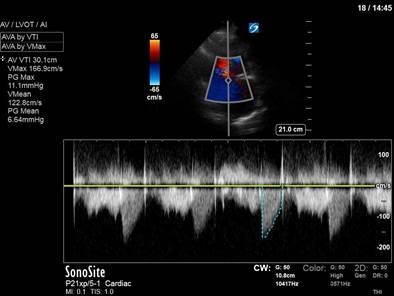
I call this one “Valve-a-palooza.” This was a 70-something woman admitted to the ICU with recurrent flash pulmonary edema. She had no previous Echo on file, and no documented prior cardiac history. However, family states that she had “a valve problem” – some family members were confident this was “a leaky valve,” while others thought “a stiff valve” was her problem. From the clips below, can you tell which valvular lesion is our clinical culprit?

Eye Scandy
An oldie but a goodie. Behold the power of a Valsalva to supersize the IJ in an upright, cooperative patient (ahem, may or may not have been yours truly). Keep this is mind next time you’re putting a CVC into a very collapsed IJ – your patient may be able to make your life much easier!
Answer to Last Weeks Case
These are clips taken with the phased-array probe of the patient’s left and right costophrenic angles, as annotated. In both clips we can see intra-abdominal organ (spleen or liver) screen right under the diaphragm, as well as a large pleural effusion with compressed atelectatic lung screen left.
In both clips, however, we also see a hyperechoic density in abutting the diaphragm near midline. The first thought is whether this could be empyema or abscess; however, note that the surrounding effusion appears fairly simple (there may be a few drifting complexities on the right side), which would not be in keeping with an empyema. The density also appears on both sides of midline, which would be unusual. So what else can inhabit the thorax? And does that right-sided well-defined hyperechoic density with a central anechoic space remind you of anything you may have seen elsewhere?
If you said stomach, you’re absolutely right. This patient had a history of a hiatal hernia, and evidence of protrusion of the gastric fundus into his thoracic cavity on a recent CT can. This is more commonly seen only on the left side, but can be located more centrally and seen bilaterally as in our patient.
The ultrasound finding had no immediate clinical implications in this case, but it’s always important to be able to identify all structures visualized on a scan, and to be able to rule out more sinister pathology.
Answer to Last Weeks COTG
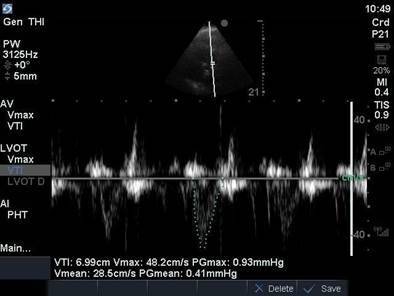
The first obvious thing here is the severely depressed LVOT VTI at 7cm (normal 18-22cm). Given a heart rate of 80 and an assumed LVOT diameter of 2cm (to quote the infamous Dany Burke – “it doesn’t have to be true, it just has to be two”), we can calculate a cardiac output of a measly 1.8L/min. Her shock, clearly, is cardiogenic in nature. But what part of the heart is to blame here?
At first glance, the contractility left ventricle may seem suspect. However, repeated viewing draws your eye to the very abnormal septal movement. Certainly in the parasternal short-axis view, the septum appears flattened and D-shaped. Closer inspection – and an ECG-gated scan would make this even more obvious – reveals marked septal flattening in diastole, and even bowing into the LV. This is so pronounced that the left ventricular cavity in the parasternal long-axis view is almost obliterated in diastole. Although some of this appearance may be due to the cylinder effect, we can doubtless say that left ventricular diastole filling is severely impaired due to abnormal septal bowing.
Overall, this represents a case of cardiogenic shock whereby left ventricular stroke volume (and therefore cardiac output) is impaired due to right ventricular failure and severe right-sided volume and pressure overload – nicely illustrating the concept of ventricular interdependence. You also get further LV impairment due to ventricular asynchrony and prolonged RV contraction.
In our patient’s case, there was known pre-existing mildly elevated right-sided pressure secondary to obstructive lung disease, with superimposed severe ARDS causing an acute rise in pulmonary vascular resistance and acute RV failure.
Attached are two articles, for those who are interested. One is a review of right ventricular failure and its management in the ICU – a good reminder given how common this clinical problem is. The other is for the true Ultranerds, courtesy of current rotator Matt White (watch this space – you’ll be hearing much more from him later in 2019 as he takes on the role of POCUS fellow!), on abnormal septal kinetics and the use of M-mode.
Happy scanning!