We’re going to take a break from Doppler this week and instead focus on the interpretation of a nice set of 2D images. Also, Katie Wiskar has returned for another 3 months of POCUS and is keen to contribute to COTW again. Stay tuned for some future posts from her as well (and perhaps the return of EyeScandy™)!
The Case
This week is a case of an 81 yo F who was admitted to the ICU after a polytrauma from an unwitnessed fall. The patient had a known history of coronary artery disease, but there was no previous echocardiogram on file. The POCUS team was therefore asked to assess his cardiac function. Have a look at the images below with a focus on the LV systolic function. What do you think? Is there anything in particular that stands out?


This is an illustrative case of clear regional wall motion abnormalities (RWMAs). In the ICU, obtaining the necessary views to confidently call RWMAs can be challenging, and it is important to avoid overcalling (and undercalling) these especially in the setting of images with poor endocardial resolution. Furthermore, to confidently call a specific RWMA, the segment of interest should ideally be seen in at least two orthogonal planes. This exemplifies the POCUS adage that one view is only hypothesis generating.
This case, however, gives very clear images at both the short axis, long axis and apical windows where we can really appreciate both the respective thickening and excursion of the different LV segments. This case also highlights the utility of the subcostal short axis views which gave much superior images compared to the associated parasternal views.
I’m going to take a quick detour to explain the foundations of the RWMA assessment. If you want to skip straight to the specifics of the case answer skip down a few paragraphs. When first starting out developing skill in LV systolic assessment the first step is simply to recognize whether the contraction pattern is homogenous or whether different areas seem to be contracting differently, called a heterogeneous pattern of contraction. With a little more practice, we can then start to appreciate the specific wall segments traditionally used in echocardiography.
Echocardiography uses a 17-wall segment classification as illustrated below (Figure from Otto’s Textbook of Clinical Echocardiography).
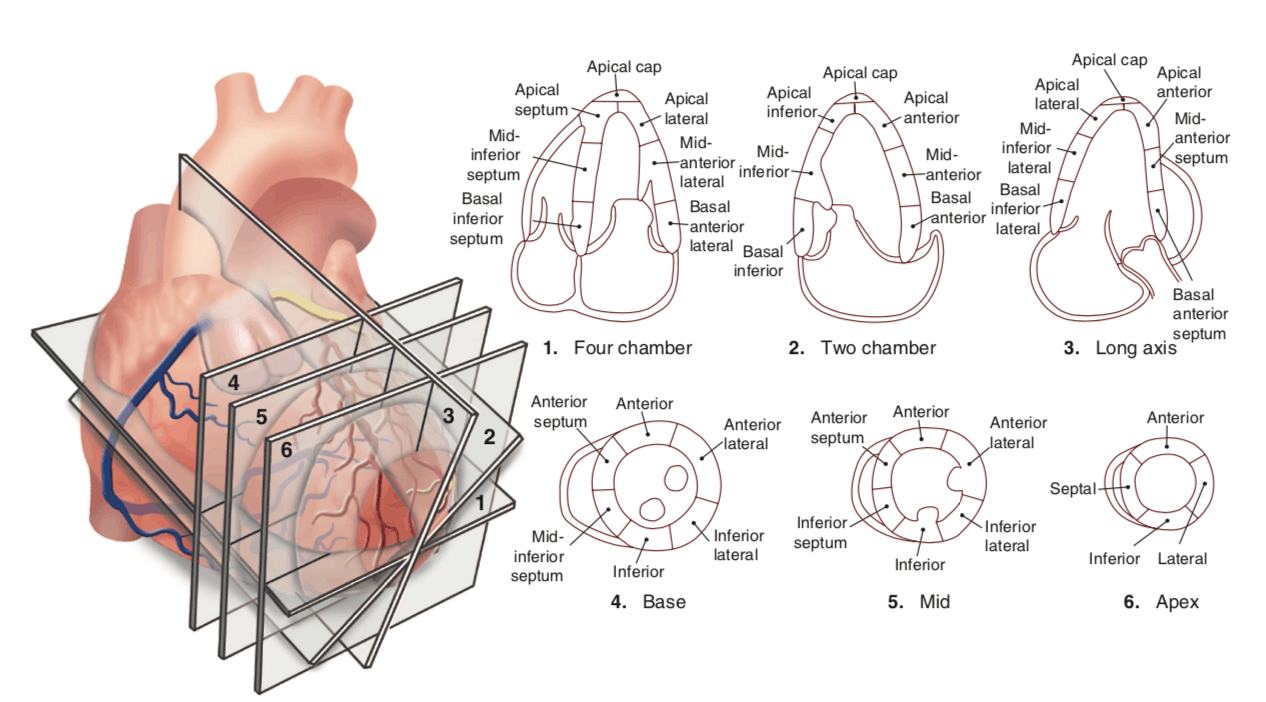
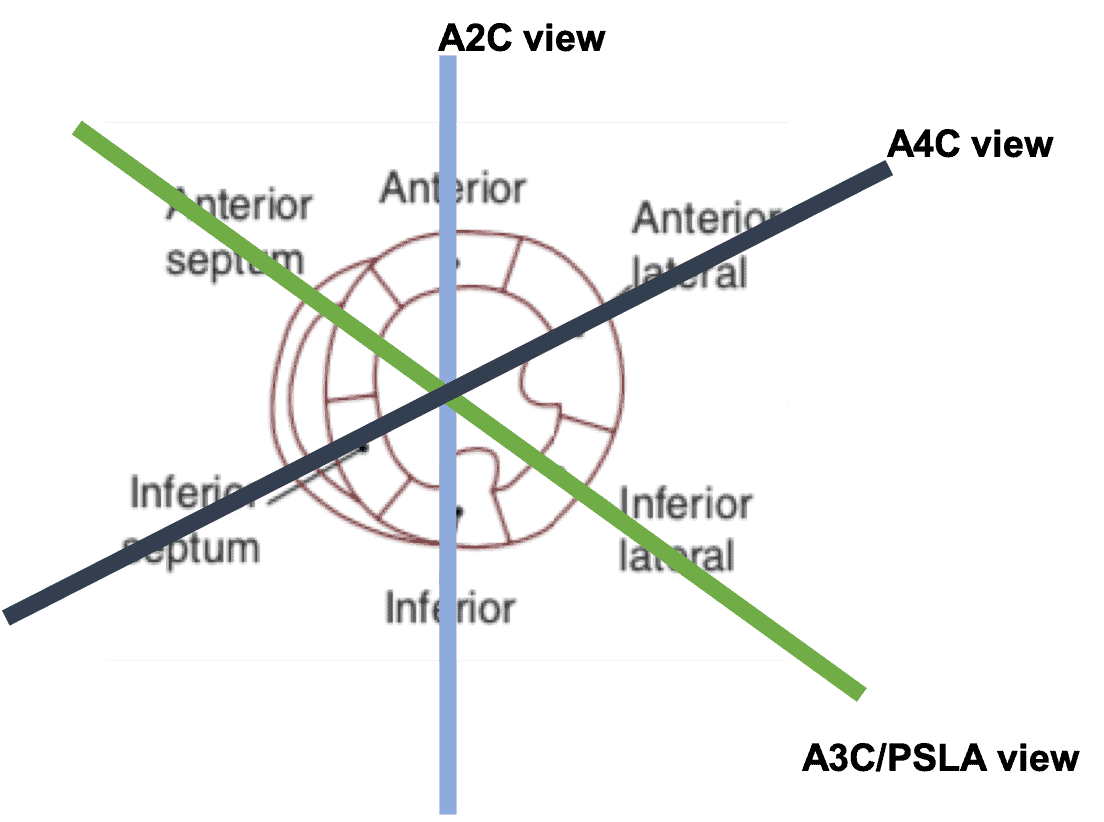
Don’t worry if this appears overwhelming on first glance. It can be really simplified by first just focusing on the trusty mid-pap level of the LV as illustrated below. At both the mid and basal levels there are 6 segments: anterior, anterolateral, inferolateral, inferior, inferoseptal and anteroseptal. Where the RV inserts on the LV (and the pap muscle) can serve as your anchor points to figure out which segment is which. So that’s 6 mid segments, and 6 basal segments so far. Some people like to simplify it a bit and use the mnemonic “SALPI” (septal, anterior, lateral, posterior and inferior). Note that some people use “posterior” and “inferolateral” interchangeably. The apex of the LV is smaller so instead of 6 different segments the apex just gets 4: septal, anterior, lateral, inferior. We’re now up to 16. The last segment is the very apex of the heart simply called the “apical cap.” As mentioned previously, we need to be examining each segment in more than one view, so we look at these segments in our other views. I’ve labeled the different cuts of the mid pap view that generate the other views (e.g. apical 4 chamber, or 2 chamber). The last aspect of assessing RWMAs is the specific grading of normal, hypokinesis, akinesis or dyskinesis.
Ultimately, what’s most important is recognizing specific patterns of RWMAs that correlate to areas of ischemia of the LAD, RCA and LCx respectively. Assessment of RWMAs can also help diagnose other cardiomyopathies such as Takutsubo’s (see the case from a few weeks ago). Below I’ve attached another figure from Otto’s Textbook of Clinical Echocardiography highlighting the different wall territories of the coronary arteries.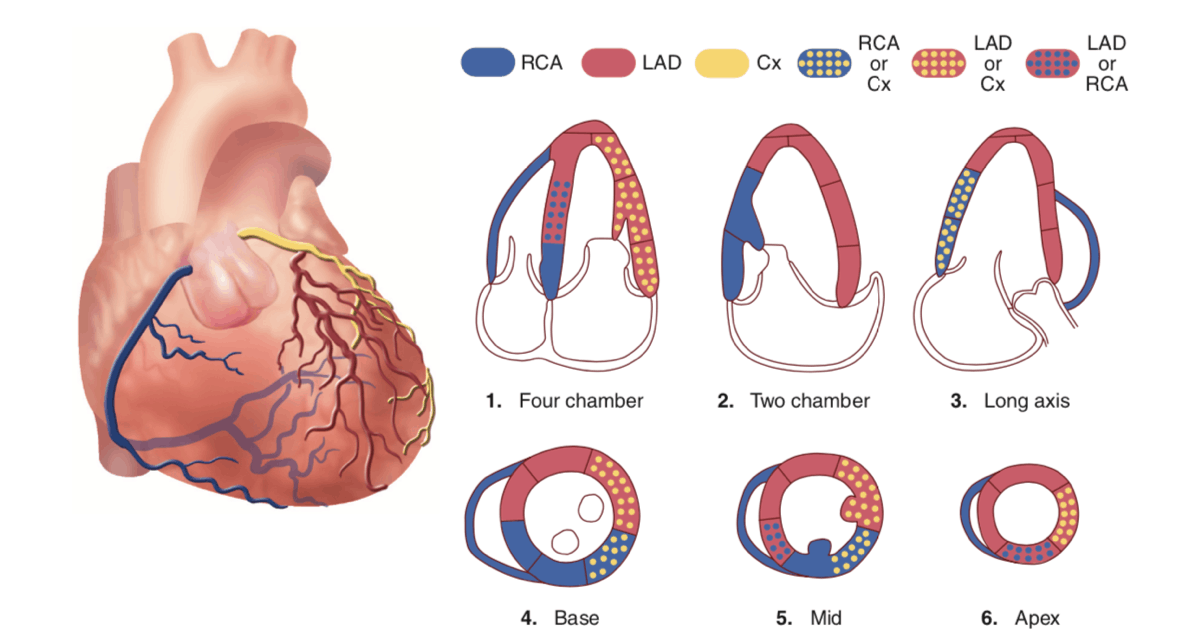
To bring it back to our case, we can see hypokinesis (and areas of akinesis, and dyskinesis) of the mid and basal inferolateral, inferior and inferoseptal walls with relative preservation of the function of the apical segments. This is most consistent with an old RCA distribution infarction. You can also perhaps appreciate some thinning of the inferior wall which is consistent with an old infarction
The last thing to note is the presence of the LV aneurysm (1.6×3.11cm) localized to the basal inferior segment seen on the apical 2 chamber view!

Given the clinical context of this case, this all fits with an old previous MI. In the more acute setting, it is important to distinguish a true aneurysm (as shown here) from a pseudoaneurysm which essentially represents a contained rupture of the free wall. Finally, an additional concern is that LV aneurysms can also provide a substrate for thrombus formation. Thus, in this case, given the presence of the LV aneurysm, a formal cardiology echocardiogram was subsequently requested which confirmed the LV aneurysm and furthermore, used contrast to exclude the presence of a LV thrombus.
Hopefully that wasn’t too much into the weeds of RWMAs! Thanks for reading!
Matt