Morning POCUS pals,
Hope you’re all gearing up to enjoy some serious hocus-pocus this Hallowe’en!
The Case
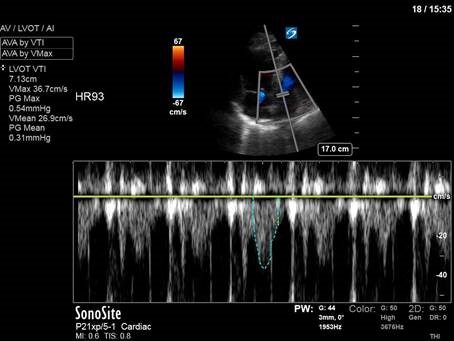
This was a 70-something gentleman who was received in the ICU after an intra-operative arrest during an orthopedic surgery for a hip fracture with an intramedullary hip screw. Given that clinical context, and the clips below, what might have occurred to cause his arrest?
COTG
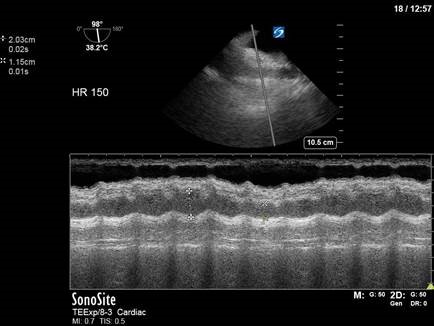
This was a peri-arrest TEE done for a middle-aged patient with profound shock NYD. From these images, is there an immediate intervention that would improve her hemodynamics?
Eye Scandy
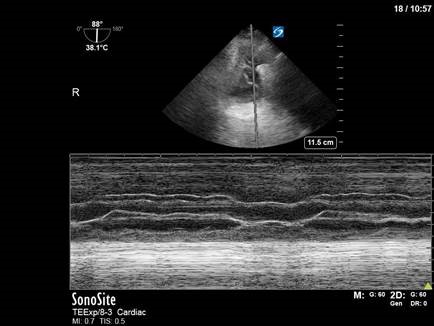
In the spirit of Hallowe’en, here are some serious cobweb-like fibrin strands seen in a small complex pleural effusion. The effusion was not well seen on traditional transthoracic lung ultrasound, but was identified using TELUS – trans-esophageal lung ultrasound. And of course, an M-mode clip – because the 8th commandment of POCUS is “If it moves, put M-mode on it.” (Full text of the POCUS commandments coming soon).
Answer to Last Weeks Case
Here we have two renal scans, both of which are abnormal.
In the first scan we can appreciate that the kidney looks markedly hyperechoic, with a thinned renal cortex and loss of the usual distinct features of the renal pyramids and renal sinus. Had we measured, we might have appreciated that the kidney was small in size as well. This is all consistent with medical renal disease – basically anything that falls under the black box of the “Renal” heading in your beloved “Pre-renal vs Renal vs Post-renal” AKI DDx. In this patient’s case, he had a recent history of membranoproliferative glomerulonephritis secondary to Hep C cryoglobulinemia vs endocarditis – diagnostic heaven for all the internists out there. (The astute among you will also have noticed trace free fluid at the inferior tip of the liver, consistent with the patient’s known ascites.)
In the second clip you can appreciate numerous rounded, anechoic structures within the kidney. While initially this may prompt consideration of hydronephrosis, closer viewing reveals that the anechoic spaces do not coalesce into a dilated renal pelvis, but are rather distinct thin-walled structures with some posterior acoustic enhancement. This is consistent with polycystic kidney disease (PCKD), which the patient was known to have.
Click edit button to change this text.
Answer to Last Weeks COTG
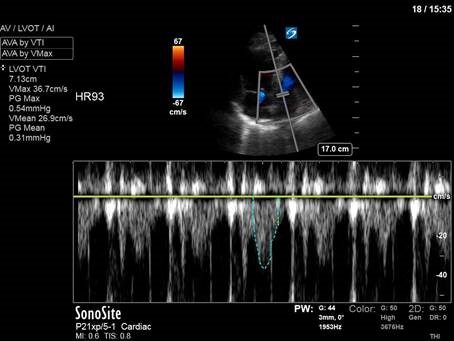
In our first clip here, we’re looking at the IVC, and can see the hepatic vein clearly tracking into the IVC, as well as the right atrium on screen right. Colour doppler has been placed over the hepatic vein, revealing high-velocity aliasing flow that appears to be bidirectional. In our second clip, we’ve placed PW over the hepatic vein in question to visualize the hepatic vein waveform.
Doppler interrogation of the hepatic vein can be useful in both liver disease and cardiac disease, as different conditions will alter the usual triphasic waveform, which should look something like this:
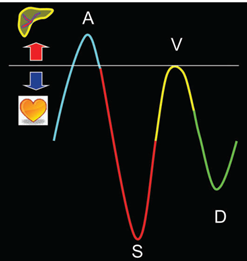
In our clip, we see a distinctly abnormal waveform with reversal of the “S” wave, which represents ventricular systole, and typically causes anterograde flow as the tricuspid annulus moves upwards and creates a negative pressure space in the right atrium, drawing blood in from the IVC. Instead, here we have retrograde flow (flow towards the liver) in ventricular systole. This is seen in severe tricuspid regurgitation, which, in this patient’s case, was caused by tricuspid valve endocarditis.

For those interested, the attached review paper provides a nice summary of hepatic waveform analysis and its use in the diagnosis of both hepatic and cardiac disease. POCUS-nerd level: very high.
That’s it for this week folks! Happy Hallowe’en, and happy scanning!
The POCUS Team





