The Case
This is a 74-year old gentleman with multiple medical comorbidities who was admitted to the ICU with septic shock and bacteremia. He’s had a tumultuous course in the unit and has been difficult to wean from vasoactive agents.
Below are two series of images. The first were taken earlier in his stay, while on higher doses of vasoactive agents and more acutely unwell. The second were taken a week later when he was clinically significantly improved and weaned from inotropic support; however, there was concerned that some of his Echo parameters had actually worsened!
What are we looking at here, and what’s the explanation?
Series A:

Series B:
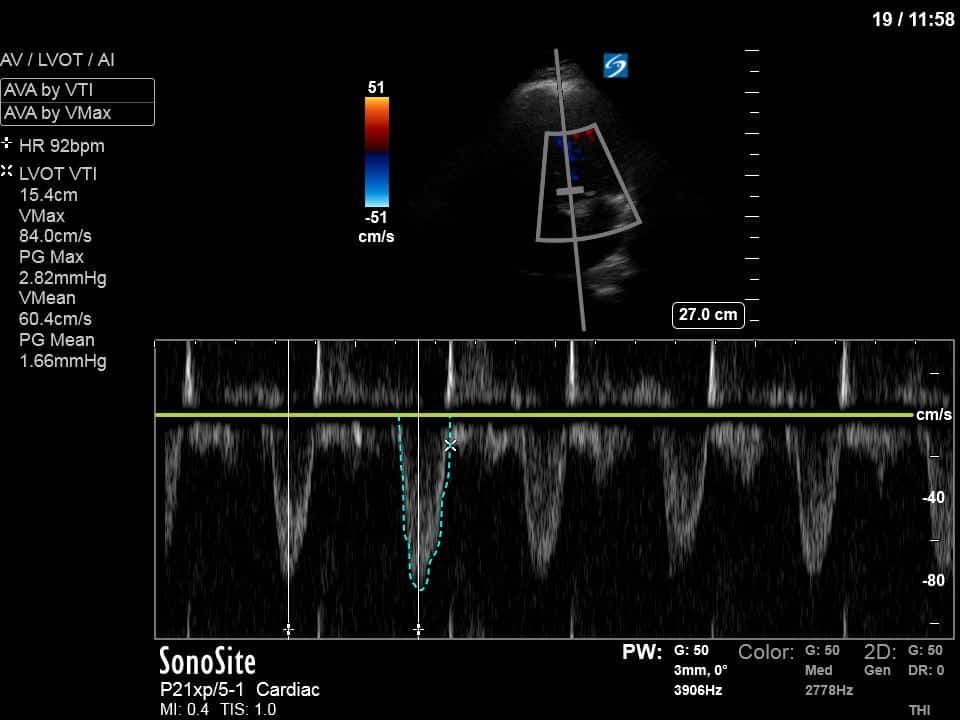
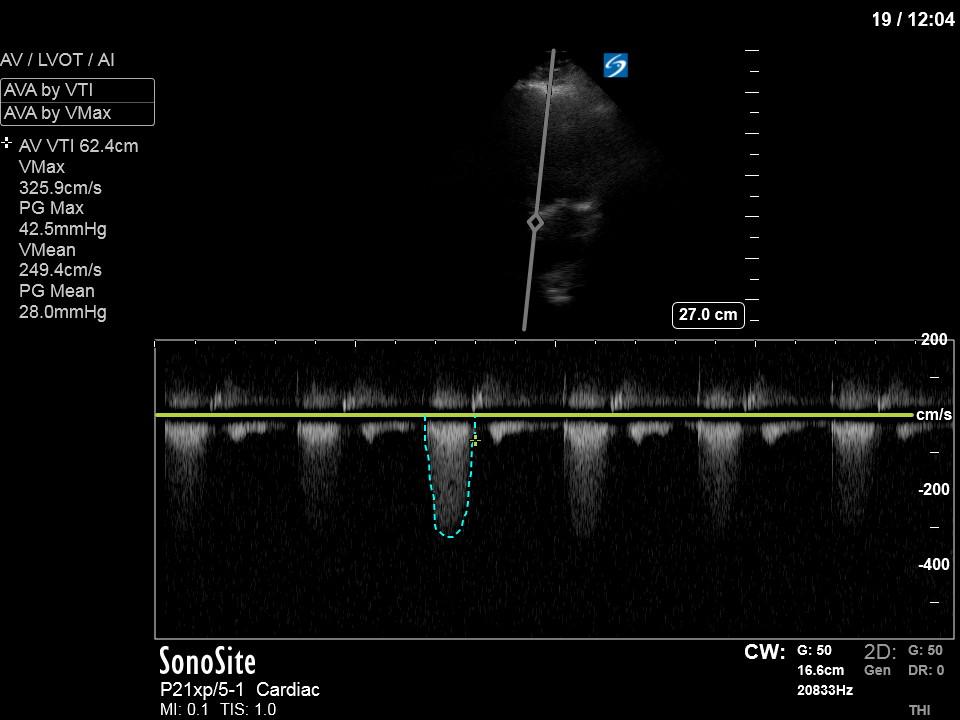
In our initial series we have a parasternal long-axis view of the heart showing reduced LV contractility, as well as a hyperechoic, calcified aortic valve that hints as possible stenotic valve disease. The following two images are spectral Doppler tracings. The first, using PW and taken in the LVOT, confirms our two-dimensional eyeball assessment of decreased LVEF, as the measured VTI is low at 15 (normal being 18-22). The second, using CW and shot through the aortic outflow tract, demonstrates aortic stenosis: we can see that our spectral waveform tracing generates a mean pressure gradient of 28mm Hg and a maximal velocity (Vmax) of 3.3m/s. The values would classify his aortic stenosis as moderate.
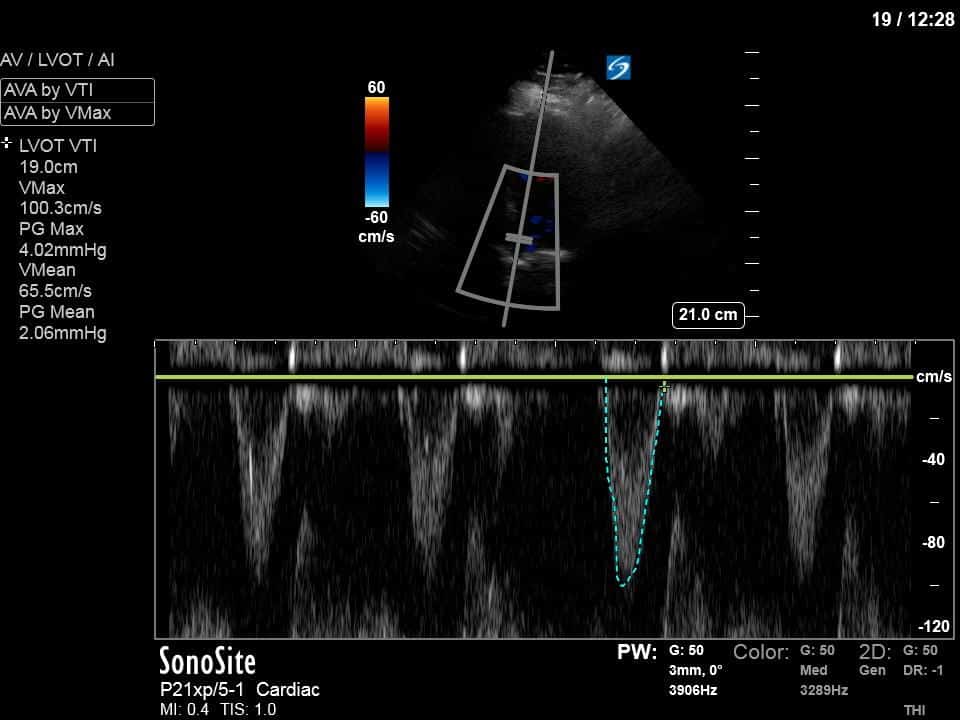
In our second series of images, we start off with an apical 4-chamber view. Although it can be difficult to compare different views (PLAX vs A4C), we get a sense that LV contractility has improved here. (You’ll also note a dilated RV with poor contractility, though we’ll focus on the left side of the heart in this case). This is confirmed by an LVOT VTI of 19, a significant improvement from previous.
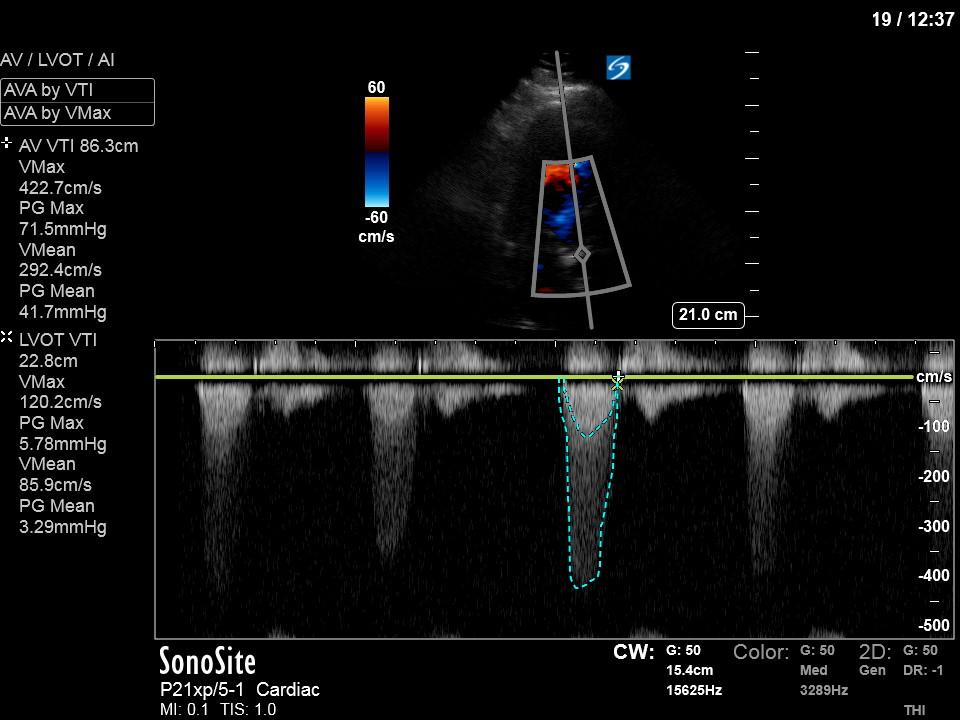
However, looking at our final image – the aortic valve VTI – it seems as though our patient’s aortic stenosis has worsened significantly in the interval between scans. He now meets criteria for severe AS, with a PG mean of 42mmHg and a Vmax of 4.2m/s. How is it possible that his valve disease has worsened so acutely?
The answer lies in the relationship between the pairs of spectral waveform tracings – that is, the relationship between the LVOT VTI (representing LV contractility) and the aortic valve VTI (the pressures generated across the aortic valve). In the first series of images, the reduced LV contractility isn’t able to generate the high pressures across the aortic valve that we typically see in severe aortic stenosis. However, with the improved contractility in the second series of images, we are now able to appreciate the true severity of the AS.
This phenomenon, as demonstrated in the first series, is called low flow-low gradient aortic stenosis. In an outpatient setting, a dobutamine Echo is often used for patients with low LVEF to see if an increase in LV contractility will reveal parameters consistent with severe aortic stenosis. In this case, the patient served as his own dobutamine Echo of sorts, with some recovery in his LVEF as his sepsis improved.
Because a dobutamine Echo is not always feasible or practical, there is another way around this problem – the Dimensionless Index. As its name would suggest, the Dimensionless Index is simply a ratio of the LVOT VTI to the aortic valve VTI, and a value of 0.25 of less is consistent with severe aortic stenosis. The DI is an ideal tool in cases like this where LV EF is reduced and you may therefore underestimate AS severity given the LV’s inability to generate high pressure gradients across a very narrow aortic valve. To calculate the DI, simply obtain and LVOT VTI (using PW) and an aortic valve VTI (using CW) as usual. These measures are typically traced from two separate waveforms, but can occasionally be captured from a single CW tracing, as demonstrated in the last picture above.
In this patient’s case, the DI in both series of images comes out to 0.25 – consistent with severe aortic stenosis.
For more on how to calculate the Dimensionless Index, see this excellent screencast from Vince Lau: https://westernsono.ca/screencasts/echo/point-of-care-hemodynamic-series/dimensionless-index/





