The Case
Our first case features a familiar foe. A young woman has been readmitted to ICU for respiratory failure. Her first stay was for right sided endocarditis due to Staphylococcus trumpus (or something like that, I may have failed my ID rotation). Her lung ultrasound suggests it may have been deported to a new home.
COTG
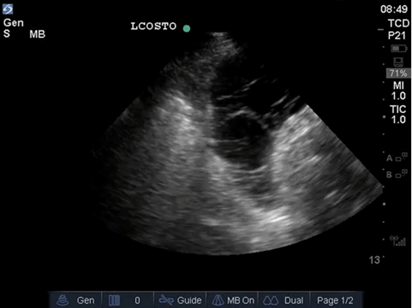
This week’s case of the geek seeks to answer a simple question, why is this patient so damn tachycardic? She’s admitted for septic shock due to peritoneal abscesses following trauma laparotomy with splenic resection and has had persistent sinus tachycardia. Fluids? Pressors? Analgesia? Sedation? Beta-blockers? What will you conclude she needs?
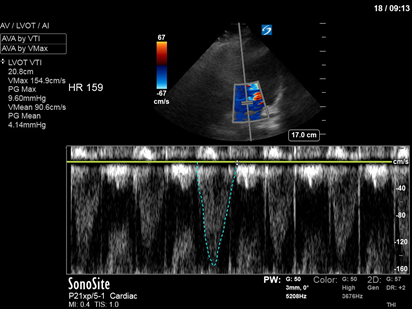
And, just for fun, here’s her short axis
Answer to Last Weeks Case

The stop still shows a D-shaped septum suggesting right ventricular failure (a common occurrence following mitral valve surgery in the Cardiac surgery ICU). The bottom clip shows a consolidated lung with static but also, more importantly, dynamic air bronchograms (the ones that flow towards the lung periphery during lung inflation (or at least attempted lung inflation)). These suggest that the lung is deflated despite air flowing through it and are highly specific for pneumonia. This is an important finding since the right lung can frequently be atelectatic following minimally invasive mitral valve surgery (it is deflated during surgery to allow surgical access and can take time to re-expand afterward). The patient was managed with antibiotics, nitric oxide to improve VQ matching and decrease RV afterload and diuresis and improved quickly. Given the RV failure and high FiO2 requirement, a bubble study was performed to rule out intracardiac right to left shunt as a contributor to the hypoxia and was negative (but you guys know all about those now).
Answer to Last Weeks COTG
The top still shows from screen left to screen right:
A consolidated lung with shred sign
The diaphragm
Weblike (damnit spiderman you’ve done it again) loculations in a fluid collection, compatible with complex ascites given it’s subdiaphragmatic location.
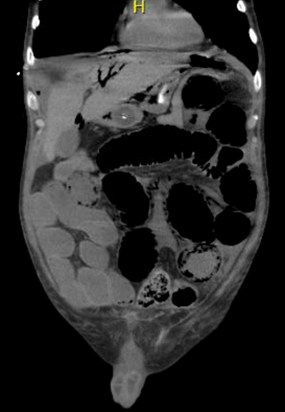
The bottom video shows dynamic air in a tissue like organ… but it’s below the diaphragm. This is the appearance of gas within the liver and, given it’s dynamic nature, suggests portal venous air rather than pneumobilia. Taken together, these findings suggest intra-abdominal catastrophe such as perforated bowel, which was shown to be the case here. And just to show we don’t play favourites, here’s the CT scan (which was obtained 4 hours later).