A tremendous Tuesday to you POCUS platoon,
Today’s POCUS lesson is sure to teach you a thing or and have you feeling as light as air. Without a further ado, let’s get at it
The Case
Our COTW comes from the Cardiac surgery recovery unit where an unfortunate sexagenarian is suffering from some hypoxemia post mitral valve repair through a right chest wall incision. His blood pressure is also having a tough go of it, with him being on Norepi 10mcg/min and Epi 6mcg/min. See if you can figure out the issue.


COTG
Our COTG comes from the medical surgical ICU where an unfortunate gentleman has been residing on/off for the past 1.5 months following an ischemic stroke. He has a history of peripheral vascular disease. He has been febrile for the past 48 hours despite broad spectrum antibiotic coverage and has developed atrial fibrillation. POCUS is asked to assess for what looks like a small pneumothorax on chest Xray. Something much more nefarious is found.
This unexpected finding’s origin is revealed by a rare POCUS gem.
Answer to Last Weeks Case
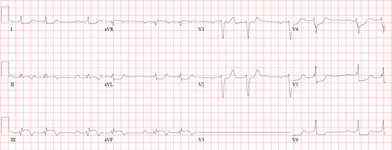
The EKG shows a pretty clear inferior ST elevation myocardial infarct. The echo shows a sluggish, dilated RV alongside some less than stellar LV function. Cardiogenic shock in the setting of an inferior MI should make you consider RV infarction as the cause. This often becomes compounded by the high vagal tone and bradycardia associated with these infarcts. Maintaining an adequate blood pressure (with pressors) is the first step to management, ensuring adequate heart rate is the next and avoiding excessive fluid overload (which is unfortunately almost universally done to RV failure given the false belief the RV just always needs more fluids) are the keys to management. See the attached article for how to appropriately manage RV failure.
Answer to Last Weeks COTG
There’s a lot to unpack from this one so let’s go methodically
What do you think of her cardiac output (her LVOT D was 1.83 and HR 65bpm):
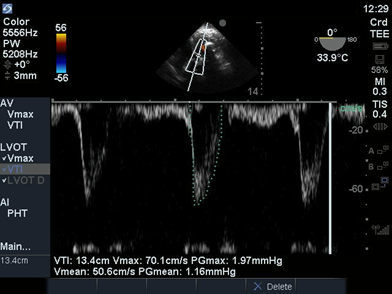
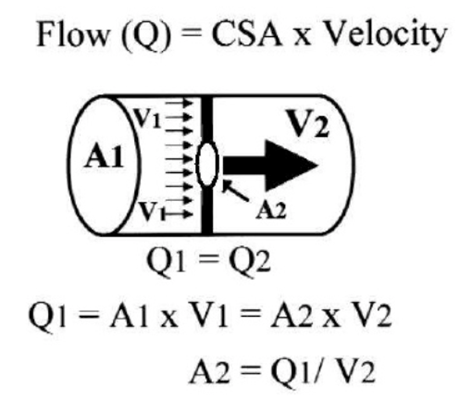
Think of stroke volume as a cylinder of fluid going through the LVOT.
It’s base area is a circle with LVOT D as it’s diameter, LVOT D/2 as it’s radius and LVOT VTI is the cylinder length
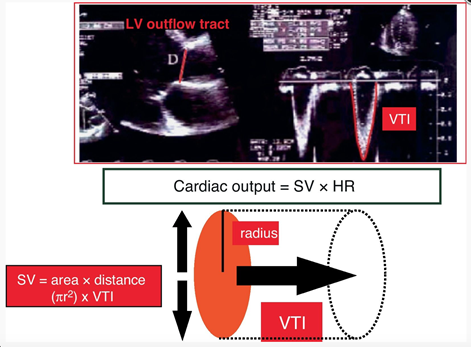
Stroke volume = pi (lvot D/2)2 x lvot VTI = 35mL
CO = SV x HR = 2.3L/min
Pretty consistent with cardiogenic shock
What do you think of her LV? Look like anything you may have with you off the coast of Japan?
That looks like a Takotsubo if ever I saw one. It is caused by an apical ballooning/dyskinesis with hypercontractility of the base which makes it look more like a great pot for catching octopus than an efficient blood pump. Apical ballooning is the best described form of stress cardiomyopathy (of which post cardiac arrest is a cause) and this is likely contributing to her poor CO.
Working our way up, how’s that MV looking? How would grade the degree of stenosis:

The opening of the mitral valve looks rather poor. However, a mean gradient of only 2.75mmHg is suggestive of only mild stenosis. But remember, pressure = flow x resistance. The resistance here is due to the Mitral valve area, which is what we’re interested in. Since her stroke volume is low (meaning low flow), the pressure will also be lower for the same valve area.
One way around this is to use the continuity equation. It’s premise is that, as long as there is no shunting of blood between cavities (as in the case of significant regurgitation or a VSD or something like that), the stroke volume going through mitral valve is the same as that going through the LVOT (and the AV for that matter). So if we know the SV through the LVOT and it’s the same as through the MV and we know the MV VTI, we can deduce the MV surface area.
so here
LVOT x lvot VTI = pi (lvot D/2)2 x lvot VTI = MVA x MV VTI
Through the magic of math we arrive at: MVA = pi (lvot D/2)2 x lvot VTI / MV VTI = 1.05cm2 , so moderate bordering on severe mitral stenosis
Have a look upstream from the MV and let us know if anything hinky is happening.
To use the appropriate term, there’s some gunk floating around her left atrium. This is the appearance of left atrial smoke or spontaneous echo contrast, more commonly seen in the left atrial appendage. It reflects a low flow, pre thrombotic state. It’s believed to be caused by low shear rates allowing the erythrocytes to cuddle up and aggregate (though nobody knows for sure because we haven’t asked them). It’s a marker of an increased risk of thromboembolic events but, interestingly, doesn’t resolve with anticoagulation since it’s a hemodynamic phenomenon.
Good job, you guys survived the mathliest COTG ever. Unlike pi, it didn’t go on forever fortunately. I’m sure only a fraction of you will find that funny. ‘Til next x – s
Dany





