The Case
This is a 54 yo M who presented with acute hypoxic respiratory failure necessitating intubation and ICU admission. Post-intubation he had a P/F ratio of 54 despite a relatively unremarkable CXR. The PEEP was increased to try to improve oxygenation. A CTPA was ordered which was negative for PE and showed just a small right lower lobe consolidation. Given that the refractory hypoxia seemed discordant with the pulmonary pathology, concern was raised for an intracardiac shunt. A point-of-care TEE was performed including a bubble study. Have a look at the selected clips below and see what you think!


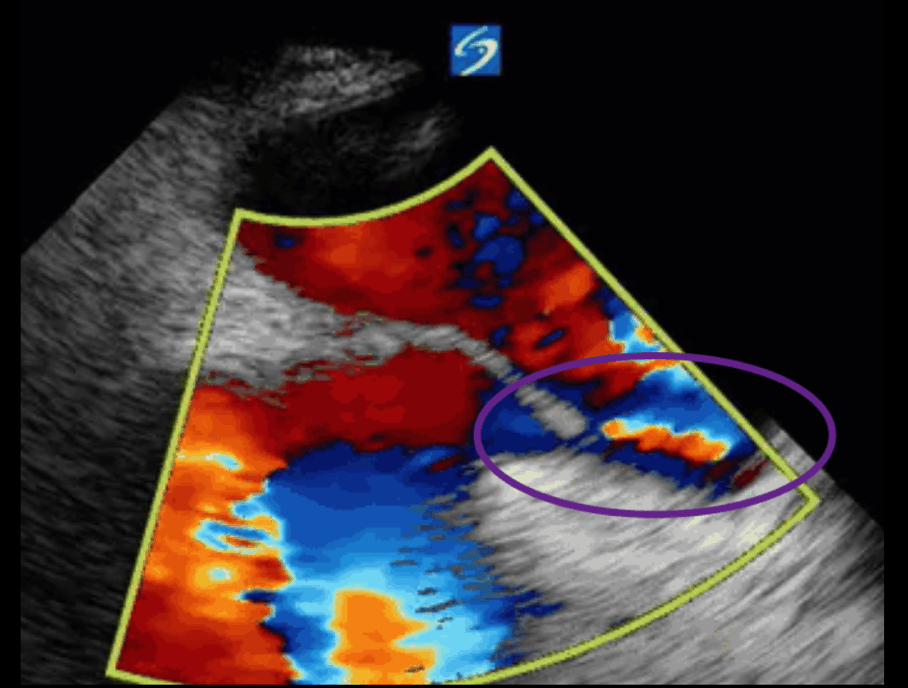
This is a positive bubble study for intracardiac shunt! To perform a bubble study using TEE the bicaval view is typically used. In this view you clearly see the LA, RA and interatrial septum. Injection of ~10cc of agitated saline allows easy visualization of a potential shunt. In this case, you can clearly see the immediate appearance of agitated saline in the LA after only 1-2 cardiac cycles. Interrogation of the interatrial septum further reveals an organized colour jet across what is likely a patent foramen ovale (PFO) and demonstrates the right to left shunt.
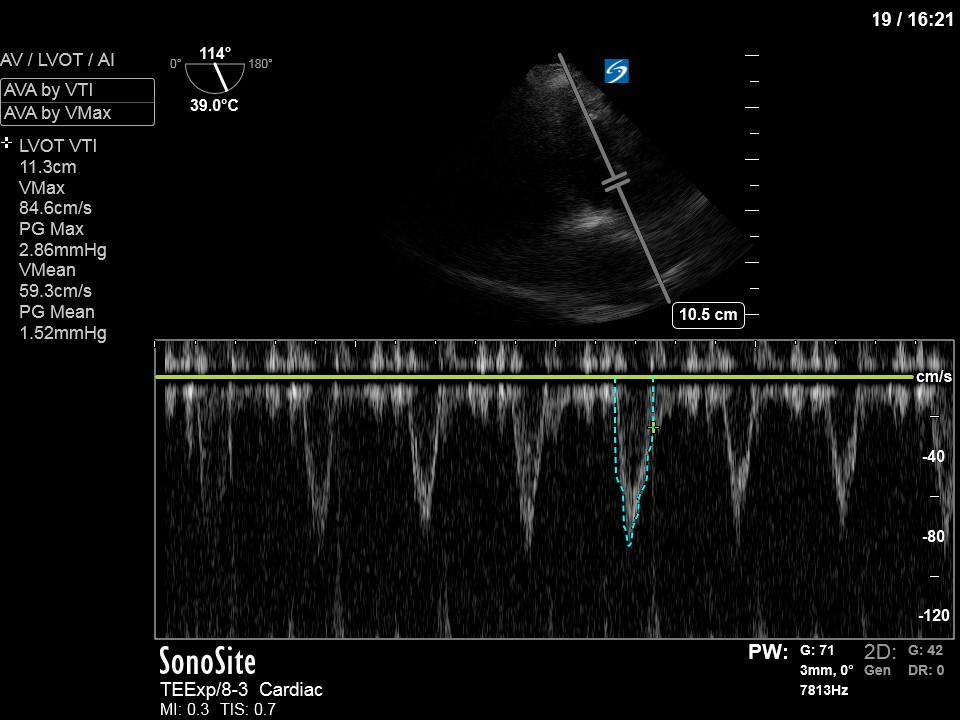
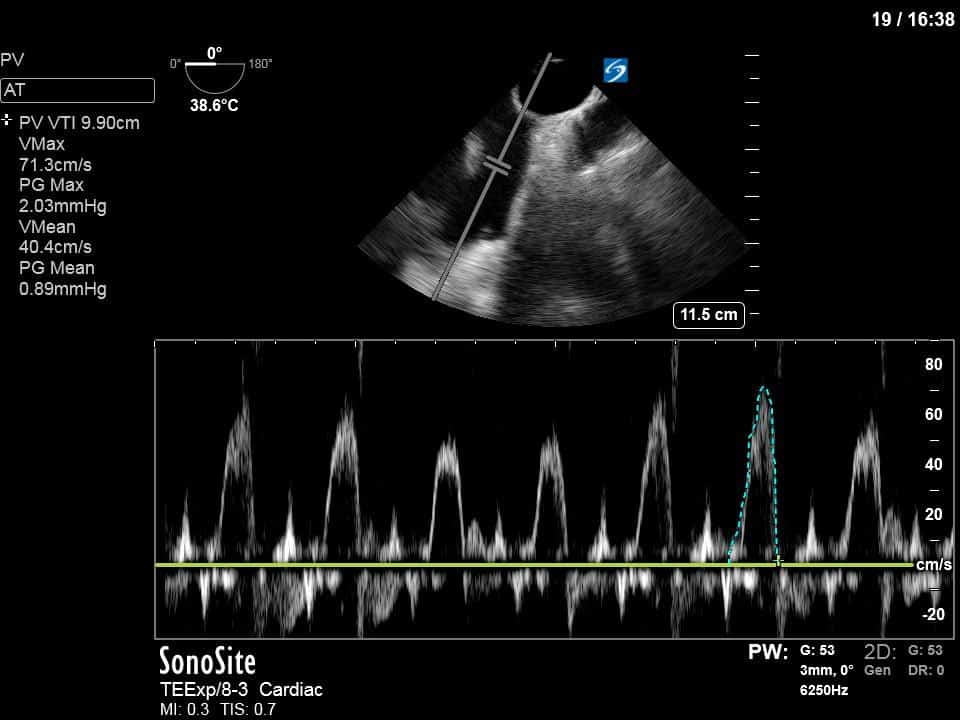
To further quantify the extent of the shunt, you can calculate the Qp:Qs – the ratio of right sided to systemic cardiac output. The calculation of Qs is the usual measurement of the LVOT VTI (see previous COTW or WesternSono screencasts for more information on this) and LVOTd to estimate the SV (and hence CO) of the LV. For Qp you apply the same principles but measure the RVOT VTI and RVOTd just before the pulmonic valve. This is best done in the mid-esophageal ascending aorta view which both gives a good view of the PV and main pulmonary artery and also allows an adequate insonating Doppler angle. In this specific case, we measured the VTI and measured the diameter in the main PA given that the RVOT was not adequately visualized in that view.
Doing the math in this case gives:
LVOT VTI = 11.4
HR 117
LVOTd = 1.93cm
CO (Qs) = (1.93/2) * VTI * 1.93
Qs = 3.9L/min
Main PA diameter = 1.84cm
Main PA VTI = 9.9cm
Qp = 3.1L/min
Qp:Qs = 3.1/3.9 = 0.8
A Qp:Qs of 0.8 essentially means that 20% of his CO is being shunted to the LV without being oxygenated by the lungs, likely greatly contributing to his refractory hypoxia. Thus, we recommended to decrease the PEEP (a counterintuitive move in hypoxia) to decrease the mean intrathoracic pressure and hopefully mitigate the right to left shunt.
Thanks for reading!
Matt






Thanks for the case. It looks like a pretty small PFO to be able to shunt that much of the cardiac output from the right to the left. If this was the case presumably the indications for PFO closure would be expanded outside cryptogenic stroke.
I’m still trying to learn, so I would be interested to hear if you agree or not.