The Case
Hi everyone!
This week is a case of a 29 yo F with known severe pulmonary hypertension. The etiology was thought secondary to cocaine-induced idiopathic pulmonary arterial hypertension. Unfortunately, she sustained a cardiac arrest (you’ll see why when you look at the images). ROSC was obtained and she was transferred to the ICU. Despite maximal medical support of her RV (optimal ventilator management, IV flolan, inhaled nitric oxide, inotropes including milrinone and vasopressin) she had persistent hypotension and worsening renal failure necessitating CRRT. The overnight team decided to trial some small boluses of crystalloid to see if that would help. Have a look at the images below and decide whether or not you would give fluids or recommend something else? If I said the CVP (as measured from the right IJ central line) was 22, what would the estimated RVSP be?

This is a case of severe RV failure! The RV is severely dilated (as is the RA) with reduced systolic function and a severely elevated estimated RVSP . In fact, this is the largest RV and highest estimated RVSP I have ever seen. Besides the obvious right sided pathology, there is also a small pericardial effusion, which is not hemodynamically relevant in this case.
There are a few things to specifically unpack here.
First, even on the PSLA view you can see the dominant RV pushing the septum inwards (especially during diastole,) crowding the LVOT. On PSSA we see the classic “D-shape” of the interventricular septum. When you see a D-shaped septum during systole only, it is suggestive of “pressure” overload. When you see it primarily during “diastole,” it is consistent with “volume” overload. It comes to no surprise, in this case, to see it during the entire cardiac cycle, consistent with both pressure and volume overload of the RV.
Furthermore, this is longstanding pulmonary hypertension, evident from the incredibly muscular and thick appearance of the RV free wall, the incredibly high right sided pressures, and finally, the concomitant severe RA dilation. The RV free wall thickness can be best measured in the subcostal view and should be less than 5mm during diastole. Although the visual appearance that the RV looks more muscular than the LV is enough, the 17mm measured confirms just how thick the RV wall is!
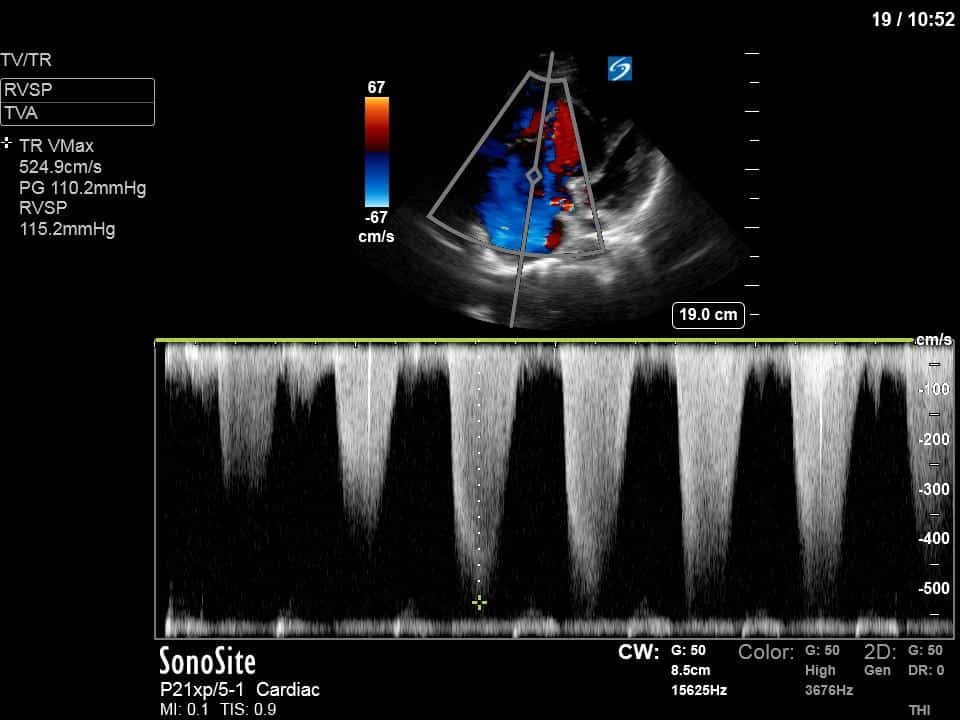
This case also demonstrates the utility of doppler to estimate the right sided pressures and provides an opportunity to go over some of the fundamentals of this. To do this we start by using colour doppler to interrogate the tricuspid valve for TR. We’re looking for a nice TR jet to then place continuous wave doppler (CWD) through it. It doesn’t have to be as severe as it is in this case (even a trace TR jet can give good spectral doppler information). As usual with doppler we want to try to align our doppler line as parallel to the flow as possible. We use CWD as the TR velocity is very high and we run into the problem of aliasing if using pulse wave doppler (PWD). With CWD we should get a nice envelope as demonstrated in this case. We can then use the peak velocity of this envelope (i.e. the peak velocity of blood flow in the regurgitant jet) to calculate the pressure gradient between the RV and the RA using the simplified Bernoulii equation (Pressure Gradient = 4v2). Once you have the pressure gradient you can then simply add the RA pressure to get an estimate of the RVSP. To understand this and the simplification of Bernoulli’s principle it’s worth checking out the following youtube video which walks you through it.
https://www.youtube.com/watch?v=cO6B9Q3At1Y
In this case, the estimated RV-RA pressure gradient was a whopping 110mmHg! Given the measured CVP of 22 (you can also estimate it using the IVC, but less reliable in ventilated ICU patients) this gives an estimated RVSP of 132mmHg!
Given the the extent of RV pressure/volume overload (the RVSP was actually higher than the LV systolic pressure), further volume would only likely worsen his hemodynamic status. Thus, the recommendation was made to actually start pulling fluid off with CRRT as a way to try to offload the RV. I have attached an article by Dr. Viellard-Baron from 2009 (it stands the test of time) which outlines the assessment of RV function in the ICU.
Thanks for reading!






Juste Amazing. Thanks for the case.