Advanced Critical Care Ultrasound Quantitative Assessment Resource
Our previous Critical Care Ultrasound Fellow, Marko Balan MD FRCPC, [...]
Best Poster at Research Day: A-LURT’ing the People on Ultrasound
The Day Last Friday I had the amazing [...]
10 Things I Learned on my POCUS Elective
"This reflective writing piece was completed by Dr. Aashish Kalani [...]
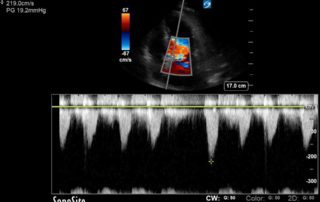
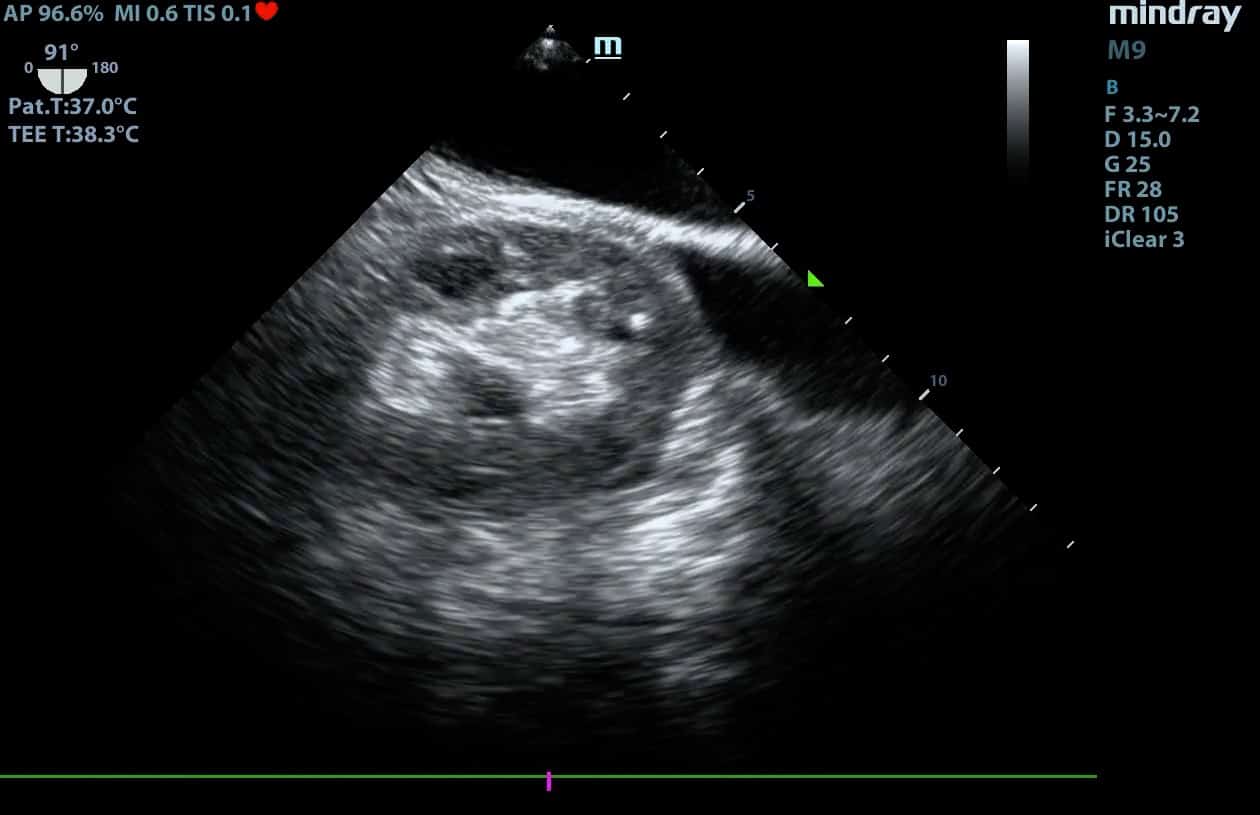
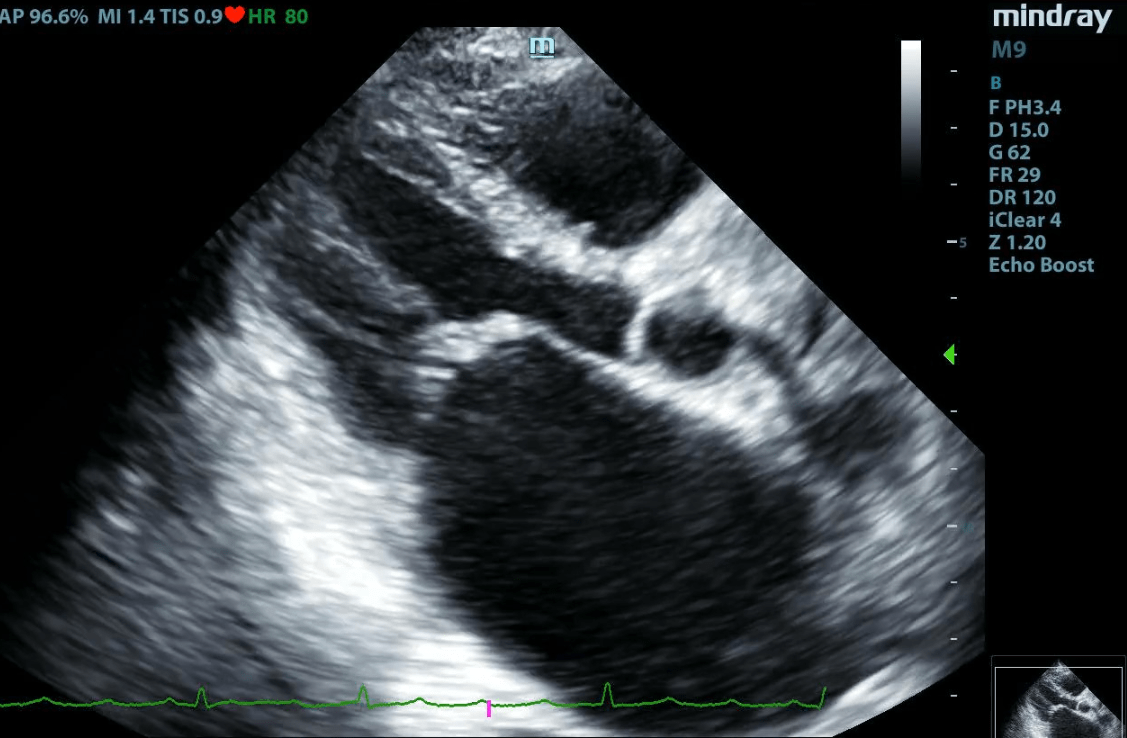
Normotensive Cardiogenic Shock Case Review
Advanced critical care echocardiography case review by Hassan [...]
Ultrasound Podcast Episode 5
Tamponade, IVC vs. Aorta, and UFO! In [...]
Ultrasound Podcast Episode 4
Role of POCUS DVT studies in different specialties, humbling [...]
Ultrasound Podcast Episode 3
Role of Point of care TEE for prosthetic valves, [...]
Ultrasound Podcast Episode 2
Surprising finding in the liver, atelectasis vs pneumonia, and introducing [...]
Ultrasound Podcast Episode 1
Welcome to WesternSono's newest project, the Ultrasound Podcast! Join us [...]