Case of the Week: October 28, 2019
This is a 74-year old gentleman with multiple medical comorbidities who was admitted to the ICU with septic shock and bacteremia. He's had a tumultuous course in the unit and has been difficult to wean from vasoactive agents. Below are two series of images. The first were taken earlier in his stay, while on higher doses of vasoactive agents and more acutely unwell. The second were taken a week later when he was clinically significantly improved and weaned from inotropic support; however, there was concerned that some of his Echo parameters had actually worsened! What are we looking at here, and what's the explanation?
Case of the Week: October 22, 2019
This is a case of a 56 yo F admitted with sepsis and MSSA bacteremia. A CT Head revealed several lesions concerning for septic emboli. She had known chronic significant mitral valve pathology documented prior to her admission. The POCUS team keen to see this pathology and to look for any additional signs of infective endocarditis. What do you notice about the valve on the 2D echo images and what specifically do you see on its colour doppler interrogation?
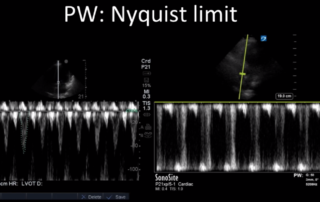
Principles of Doppler
Principles of Doppler Learn the principles of Doppler ultrasound [...]
Case of the Week: October 15, 2019
This is a 78-year old woman admitted a week prior with respiratory failure secondary to CHF exacerbation and COPD; on admission, she had a pleural effusion that was tapped and found to be transudative. She now has ongoing dyspnea in the ICU with increasing oxygen requirements. so the POCUS team was called in to help sort things out.
Case of the Week: October 2, 2019
81F admitted to ICU after polytrauma from an unwitnessed fall. Known history of coronary artery disease, but no previous echocardiogram on file. The POCUS team was therefore asked to assess his cardiac function. Have a look at the images below with a focus on the LV systolic function. What do you think? Is there anything in particular that stands out?
Case of the Week: September 18, 2019
This week is a case of a 29 yo F with known severe pulmonary hypertension. The etiology was thought secondary to cocaine-induced idiopathic pulmonary arterial hypertension. Unfortunately, she sustained a cardiac arrest (you’ll see why when you look at the images). ROSC was obtained and she was transferred to the ICU. Despite maximal medical support of her RV (optimal ventilator management, IV flolan, inhaled nitric oxide, inotropes including milrinone and vasopressin) she had persistent hypotension and worsening renal failure necessitating CRRT. The overnight team decided to trial some small boluses of crystalloid to see if that would help. Have a look at the images below and decide whether or not you would give fluids or recommend something else? If I said the CVP (as measured from the right IJ central line) was 22, what would the estimated RVSP be?