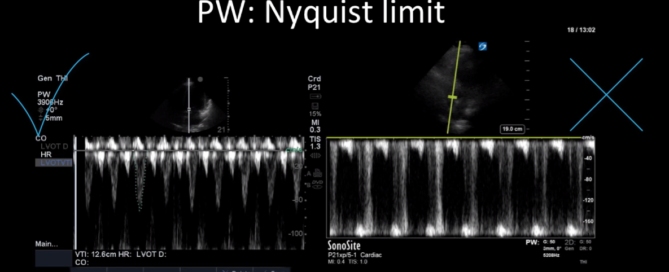
Case of the Week: November 11, 2019
This is a 40-year old man status post-liver transplant (several months prior) who has had a complicated hospital course. He is now re-admitted with presumed septic shock (query HAP) and has been intubated for respiratory failure. He's also had a formal abdominal ultrasound commenting on periportal hepatic edema and signs of congestion. Based on the images below what interventions might you make to the team in addition to antimicrobial therapy? The team is particularly worried about right heart failure and elevated right-sided pressures - what do you tell them based on your findings?